Table of Contents
PREFACE TO THE 15TH EDITIO
CHAIRMAN’S WELCOME
RESIDENCY DIRECTOR’S WELCOME
Vision Statement
ACGME CORE COMPETENCIES
KCH ED
KCHC Main ED Junior Resident Clinical Role
KCH Senior Resident Clinical Role (Main ED)
Pre-attending Role
KCH PEDICATRIC EMERGENCY DEPARTMENT
KCHC Pediatric ED Resident Clinical Role
UHB EMERGENCY SERVICES
UHB Junior Resident Clinical Role
UHB Senior Resident Clinical Role
UHB “Resident in Charge” Clinical Role
EDUCATIONAL OBJECTIVES
EDUCATIONAL OBJECTIVES – PGY 1
EDUCATIONAL OBJECTIVES – PGY 2
EDUCATIONAL OBJECTIVES – PGY 3
EDUCATIONAL OBJECTIVES – PGY 2
OFF SERVICE ROTATIONS
PGY-1 OFF SERVICE ROTATIONS
JUNIOR ULTRASOUND ROTATION
ED-BASED TRAUMA
OBSTETRICS
MICU
INTERNAL MEDICINE FLOORS AT KCH
PGY-2 OFF SERVICE ROTATIONS
AIRWAY MANAGEMENT
CCU
NICU
ENT
SICU
Stroke
Emergency Orthopedic/Fast Track Rotation
PGY-3 OFF SERVICE ROTATIONS
EMS
TOXICOLOGY
RESEARCH
EMERGENCY ULTRASOUND ROTATION
PGY-4 OFF SERVICE ROTATIONS
ELECTIVE
ELECTIVE PLANNER WORKSHEET
International Elective Curriculum
MEDICO-LEGAL
MEDICAL EXAMINER
DERMATOLOGY
ORAL SURGERY
Administration Rotation
EDUCATION
READING
MODEL OF CLINICAL PRACTICE OF EM
IN-SERVICE EXAMINATION
BOARD REVIEW GROUP
EMERGENCY MEDICINE BOARD EXAMINATION
USMLE EXAMINATION REQUIREMENTS
MORNING REPORT
WEDNESDAY CONFERENCE
ED CONFERENCE ATTENDANCE POLICY
INDEPENDENT STUDY
PRESENTATION PREPERATION POLICY
SENIOR RESIDENT LECTURES
MISCELLANEOUS POLICIES AND PROCEDURES
RESIDENT RESPONSIBILITIES AND DUTIES
Policy on Eligibility and Selection of Residents
PROMOTION/GRADUATION CRITERIA
Supervision of Residents and Escalation Policy
POLICY ON RESIDENT WORK HOURS
CLINICAL PROCEDURES
EVALUATIONS and FEEDBACK
RESIDENT PORTFOLIO
Quality Improvement (QI) Project
Pay line switching
TRAVEL PLANS & REIMBURSEMENT PROCEDURES
GME Due Process Policy
GME Academic Performance Due Process Policy
GME Misconduct Due Process Policy
FACULTY ADVISOR8
SICK CALL POLICY
Sick Call Procedure: KCH and UHB ED
Sick Call Procedure: Off-service and Affiliate EDs
Sick Call Procedure Conference Days
ED CONFERENCE ATTENDANCE POLICY
Missed Requirements Policy
WORK ATTIRE POLICY
MOONLIGHTING
POLICY ON CHIEF RESIDENT SELECTION
ON CALL ROOMS AT KCHC
EMPLOYEE HEALTH SERVICE (EHS)
NEEDLESTICK/BODY FLUID EXPOSURE PROTOCOL
Institutional Policy ON DISCRIMINATION & SEXUAL HARASSMENT
FAMILY MEDICAL LEAVE ACT
THE IMPAIRED PHYSICIAN
Emergency/Disaster Preparedness 2013-2014
STUDENT EDUCATION
ONLINE RESOURCES / CIS / INTERNET / EMAIL / TECHNOLOGY
MONTHLY SCHEDULES
PREFACE TO THE 15TH EDITION
Welcome to the updated 2013 Edition of our Emergency Medicine Residency Handbook!
Please read this handbook carefully since it contains information about the residency, our Department, the affiliates, various rotations, protocols, guidelines, and policies.
This handbook was written not only for the residents, but also for faculty members, attendings, students and anybody involved in our department. It contains vital information for the smooth operation of the department and successful completion of your residency.
We would like to thank everyone who has contributed to this new edition. Please feel free to contact us about any discrepancies, questions, comments and suggestions.
It is important that you read through the handbook carefully. As always, several changes have been initiated. Please note changes in policies, rotations and affiliates. We have decided to publish the handbook in a loose-leaf format. As changes occur in the future, you will be able to pull old sections out and replace them with updated information. In addition, we have published this edition on the web under the following web address:
http://www.downstate.edu/emergency_medicine
We wish you the best of luck!
Stephan Rinnert, MD Mark Silverberg, MD
Residency Director Associate Residency Director
Antonia Quinn, DO Teresa Smith, MD
Assistant Residency Director Assistant Residency Director
Jay Khadpe, MD James Willis, MD
Assistant Residency Director Assistant Residency Director
Claritza Rios, MD
EM/IM Residency Co-Director
CHAIRMAN’S WELCOME
Welcome! We are all very pleased that you will be spending the next four or five years of your career in the Emergency Department of SUNY-Brooklyn at Kings County Hospital. You have chosen to train at one of the busiest Emergency Departments in the country. We are a full academic department (1 of 61 in the country). Our residents rotate through four of the twenty-one affiliated emergency departments in the SUNY-Brooklyn system. While rotating through these facilities, you will be working with the finest emergency medicine physicians in the New York City area. The combined census for these four emergency departments is nearly 550,000 patients/year, more than double of any other residency program in the nation. You will be exposed to an arena of pathology rivaled by no other program in the United States. From the critical care and infectious disease, to the cardiovascular disease, as well as an unparalleled community hospital experience in Kings County and University Hospital of Brooklyn, you will “see…do…then teach”, as your peers merely read.
This does not come without a price. I expect you to work hard, be a caring physician, and to teach. As a resident in one of the finest university systems in the country, you have the responsibility to teach your colleagues, your students, your staff and your patients. Our goal is to turn you into academicians and lifetime teachers. We are looking to train the future leaders in the field of emergency medicine.
I look forward to our bedside presentations, lively discussions at Wednesday conference and searches for the diagnosis at 2am. We, together are about to grow… it’s the reason why I’m here.
Welcome, and good luck.
Michael P. Lucchesi, M.D
Chairman of Emergency Medicine
Chief Medical Officer, UHB
RESIDENCY DIRECTOR’S WELCOME
Welcome to the Combined EM-IM & Categorical Emergency Medicine Residency at SUNY Downstate Medical Center/Kings County Hospital and its affiliates.
The faculty and I believe that this residency will provide the best and strongest learning environments in the field of Emergency Medicine. My job as program director is to be the facilitator and guarantor on your way to becoming a superb Emergency Physician. Your role shall be that of a professional, with a desire to learn while providing excellent and compassionate care. Residency is not always an easy strait to travel and there are a myriad of obstacles to navigate before reaching the final destination. We will do this together. Let us be always mindful of the fact that we must keep high expectations of ourselves and others; this will lead us to be ever-working to achieve excellence of ourselves and for our patients.
This resident’s handbook shall serve as one of the roadmaps on your travel to success. It contains many useful tips as well as some very basic rules. Please read the manual carefully. It is implied that by signing a receipt for this book that you are familiar with its content.
I wish you success in your residency as a starting point of a wonderful and fulfilling career.
Stephan Rinnert, MD
Associate Professor of Clinical Emergency Medicine
Vice Chairman for Education and Faculty Development
Residency Program Director
Department of Emergency Medicine
Adjunct Associate Professor School of Public Health
SUNY Downstate / Kings County Hospital
Brooklyn, NY
Vision Statement
The residents in the program will be leaders in the department, leaders in the university, leaders in the community, and eventually leaders in Emergency Medicine. We will be a culturally aware and ethnically diverse center of excellence in Emergency Medicine education. The overall goal of this program is to provide outstanding and compassionate patient care while fostering critical thinking and curiosity as well as implementing advances in the care of the emergency patient. We will strive to transform our residents into role models in the provision of patient-centered healthcare beyond our own institution but with a global reach.
Work Environment
The department will create an environment for our residents that is conducive to learning; intellectually stimulating; personally satisfying; safe from physical and emotional harm; and free of discrimination based on the residents’ sexual orientation, spiritual beliefs, race, ethnicity, identified gender, or socioeconomic background.
ACGME CORE COMPETENCIES
Criteria by which residents’ performance will be judged is outlined below:
PATIENT CARE (PC)
Residents must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Residents are expected to:
- Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients and their families
- Gather essential and accurate information about their patients
- Make informed decisions about diagnostic and therapeutic interventions based on patient information and preferences, up-to-date scientific evidence, and clinical judgment
- Develop and carry out patient management plans
- Counsel and educate patients and their families
- Use information technology to support patient care decisions and patient education
- Perform competently all medical and invasive procedures considered essential for the area of practice
- Provide health care services aimed at preventing health problems or maintaining health
- Work with health care professionals, including those from other disciplines, to provide patient-focused care
MEDICAL KNOWLEDGE (MK)
Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to clinical decision making. Residents are expected to:
- Demonstrate analytic thinking and a systematic approach to clinical situations
- Know and apply the basic and clinically supportive sciences that are appropriate to the Emergency Dept.
- Develop an appropriate differential diagnosis.
PRACTICE-BASED LEARNING AND IMPROVEMENT (PBL)
Residents must be able to investigate and to evaluate their patient care practices, appraise and assimilate scientific evidence, and improve their patient care practices. Residents are expected to:
- Analyze practice experience and perform practice-based improvement activities using a systematic methodology
- Locate, appraise, and assimilate evidence from scientific studies related to their patients’ health problems
- Obtain and use information about their own population of patients and the larger population from which their patients are drawn
- Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness
- Use information technology to manage information, access on-line medical information; and support their own education
- Facilitate the learning of students and other health care professionals
INTERPERSONAL AND COMMUNICATION SKILLS (C)
Residents must be able to demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, their patients families, and professional associates. Residents are expected to:
- Create and sustain a trusting and effective relationship with patients and family members
- Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills
- Work effectively with others as a member or leader of the health care team
PROFESSIONALISM (P)
Residents must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. Residents are expected to:
- Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supersedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development
- Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices
- Demonstrate sensitivity and responsiveness to patients’ culture, age, gender, and disabilities
SYSTEMS-BASED PRACTICE (SBP)
Residents must demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value. Residents are expected to:
- Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and the larger society and how these elements of the system affect their own practice
- Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources
- Practice cost-effective health care and resource allocation that does not compromise quality of care
- Advocate for quality patient care and assist patients in dealing with system complexities
- Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance
KCH ED
- Introduction
Welcome to the Kings County Hospital Center Emergency Department. At over 135,000 patient visits per year, it is one of the largest Emergency Departments in the country. This patient volume and the high acuity will serve as the classroom for one of the most hands-on, educational experiences you will have during your training. When you start your first clinical shift, you should ask the senior resident for a tour of the ED and a description of the available resources and supplies.
Our E.D. is subdivided into several areas based upon triage and patient age:
- CCT – Critical Care and Trauma
- Main ED aka Suite A/B – General medical/surgical illness/obstetrics/ gynecology
- Pediatrics
- Fast Track
- CCT-Critical Care Trauma
This area is what makes your residency experience at Kings County so special. It is essentially an ICU based in the ED where the most acute patients are stabilized and treated. This includes both medical and trauma patients. One attending with a senior and junior resident staffs the CCT. You will be expected to perform procedures including but not limited to lumbar punctures, central lines, CVP lines, and arterial lines. There is good nursing staffing and a PCT in the CCT but be expected to put in IV lines if the patient is in extremis. Juniors, it is expected of you to arrive to your shift at least 15 to 20 minutes early to check the resuscitation bay and stock your airway equipment and IV equipment, and make sure you are ready to handle anything that comes in. Use your time in the CCT to learn from your attendings, seniors, and patients.
- Main Adult ED – Suite A/B
The majority of your KCH Adult ED shifts will be here. The cases you will encounter here will challenge your knowledge of basic medicine and recognition of potential emergencies, such as acute myocardial infarction, pulmonary embolism, diabetic ketoacidosis, sickle cell crisis, and impending respiratory failure in asthmatics. You will experience a good degree of independence. Reading for this area should be focused on interesting cases that you see. Our advice is to pick one topic each day to review or learn, based on what you saw during your shift.
Suite A/B is divided into a quad system, geographic mapping of the ED into 4 regions. Each region consists of resident(s), 2-3 nurses and 1-2 PCT/PCAs. Depending on the amount of staff on a given day there maybe one or more residents assigned to a Quad. Quads 1-2 are located next to the main entrance while Quads 3-4 are situated towards the back next to radiology. The hallways in main ED have been labeled to facilitate patient identification and location. There is usually one attending physician for each half of main ED (Quads 1-2 and Quads 3-4). The Quad assignments are usually emailed to the class 2 weeks in advance. If at any time you have a question about the Quad system or you proper assignment you can always ask the senior in your area and they will guide you accordingly.
Residents are to work, round and sign-out only in their assigned quad area. The attending must closely monitor sign-outs by junior or rotating residents. Residents and attendings are not supposed to call pts into the ED. If you are ready to see a pt, and the next patient is in the waiting room, discuss this with the charge nurse or flow nurse. When there are 3 attendings, the third attending should function as a “float” attending. Preferably this attending should look to help out a quad that is behind in terms of wait times. They should also look to help out a quad that has a non-EM resident. The senior resident, at times and in discretion with the attending, may switch around junior and rotating residents when one or more Quads are busier than others when staffing permits. Please introduce yourselves to your “team” members on your team (i.e. nurse, PCA/PCT). Ask them when they are taking their breaks and who will be covering them.
In the main ED, there are usually several nurses, patient care associates PCAs, patient care technicians (PCTS), physician assistants, and a respiratory therapist, who will cover the asthma room during the day. You may be responsible for IVs and blood work, however we now have dedicated phlebotomists. ECGs and patient transport to X-Ray are the PCTs’ responsibility, but it may be necessary to assist with these tasks as well. If you require blood draws, order the lab tests in the computer “as phlebotomy draw stat”. In regards to imaging, the CT and x-ray transporters will come and pick up your patient when they are ready to perform the study.
Teaching opportunities by the attending staff is abundant in this area. Please ask questions! This is an excellent time to learn from the attending staff, many of who have sub-specialized in various areas of medicine. You will be asked questions about your choice of management during sign out rounds, so make sure you know why you are managing a patient a certain way. Also, challenge yourself to practice your differential diagnosis skills.
- FAST Track - as part of the ortho/FT rotation
A day in the Fast track, as with other areas of the department, starts off with sign out rounds. Although done a bit informally, as compared to its counterparts. The fast track area offers an excellent opportunity to manage minor trauma, laceration repair, I&D, orthopedics, ophthalmology and countless gynecological cases. You will be given a great deal of independence in this area and the majority of your cases will be managed to completion. The fast track may be one of our less acute areas; however, don't be fooled, many times very sick patients present there.
If needed, expect to do all blood draws in this area. In addition, you may need to get or deliver your patient to X-Ray and CT scan to expedite matters. There is usually a PCT assigned Fast Track and the tech will be the one to accompany the patients that need evaluation at other areas of the hospital (i.e. for official sonography,). There is only one nurse assigned to this area and he/she will administer all medications. If consultations are needed, phone the page operator at x3141, give her the requesting service and your call back number. Once you and the attending have reached a disposition, you can ask the clerk to schedule an appointment if the patient is being discharged or put the patient in for admission.
Morning Report: Morning report is the opportunity for our department to discuss cases in a more formalized manner. This conference is held after morning rounds on Mondays, Tuesdays, Thursdays, and Fridays. Senior residents will present a case for discussion. Attendance is mandatory for all residents working the day shift and residents who worked the previous overnight shift.
Wednesday Conference: Conference for EM residents will be held each Wednesday in the department conference room, unless posted otherwise. Attendance is mandatory. The conference is composed of various didactic lectures covering the core curriculum of Emergency Medicine, specialized case discussions pertaining to Pediatrics, the MICU, Trauma, Journal club, morbidity and mortality conference, a CPC, and monthly grand rounds.
Sign Outs: If you are leaving the ED for lunch, lecture or at the end of your shift, all patients assigned to you must be signed out. The attending that has reviewed the patient with you should be aware that you are leaving. Always inform the most senior person if you are leaving the clinical area.
- Consults
Specialty consultations are available in all services. All consults must be ordered in the computer. If, as the Resident Physician, you are having difficulty contacting a given service, you are to discuss this immediately with the attending of record for the case. OB-GYN consultation for pregnant patients less than 20 weeks will take place in the ED in Suite A/B. All pregnant patients greater than 20 weeks who arrive via EMS must first be triaged in the ED, if they are ambulatory they can be guided directly to S5 (L&D).
At the time it is determined that a patient requires general admission to the hospital, you must discuss the case with an attending physician. The nurse should be notified of the admission. Complete a “disposition note” in the Quadramed system once the decision to admit has been reached. This will place the patient on the bed board and notify admitting so that a bed can be procured. All medical admissions are then discussed with the medical senior who will call in the admission to the floor team. All admissions to the ICU or another specialty service must first be discussed with the appropriate contact person.
- Radiology Services
The Department of Radiology provides full-service radiological services. Please be aware that CTs do not need to be approved by the radiologist before the technician will perform them. Preliminary readings of films may be obtained by the radiology resident by calling or walking over to the radiology department (x1406). All plain films are to be reviewed by yourself and the Attending Physician of record on the PACS system, located on each computer. The radiology senior should be contacted via the UHB page operator (270-2121) to discuss all off-hour specialty studies, i.e. ultrasound.
Currently, we utilize QuadraMed for electronic charting, order entry and results review. Please become familiar with it. It is expected that you will complete the patient chart, providing all pertinent historical, physical, and laboratory/radiological/EKG interpretive information—both positive and negative—prior to patient disposition. History, physical exam, and initial assessment and plan should be documented in the ED Provider Initial Note. The ED Quick Note can be used to report pertinent lab or imaging results and reassessments. The final disposition, admission verse discharge, is done in the Disposition Note.
If a patient is to be discharged, all patients must have specific discharge instructions, including time and place of follow up appointments, return instructions, and any medication/care instructions. Micromedex Aftercare Instructions and Krames Educational Materials are available for discharge instructions.
- Follow-up Appointments
Follow up appointments can be obtained by asking the clerk in your area. The general clinic appointment number is 245-3325. The disposition note in Quadramed also has an area for documenting follow-up appointments.
- Clinical Schedule
The Scheduling Chief Resident is responsible for the making and distribution of the monthly KCH ED schedule. The Chief Resident on-call is the most important person with respect to the intricacies of the daily schedule and is the first person to approach with scheduling questions and requests. All schedule changes must be approved by Chief Resident on-call. The following is a brief outline of policies related to the monthly schedule.
- Any late requests will not be accepted.
- Please check the schedule, even if you requested certain days off. Requests are not guaranteed, but every effort will be made to honor them.
Please refer to the “Resident Schedule” section for details.
- Educational Objectives
- Emphasis will be placed on orientation to the different emergency department environments. Residents should learn to document a chart appropriately (C,PC,MK,P), prioritize and organize activities, perform basic procedural skills, work with EMS(C,P,PC), deal with friends and families of patients (particularly those who are critically ill or dying (P,PC,C,SBP) and deliver quality patient care(P,PC,MK). The resident should demonstrate accurate and appropriate history and physical exam skills, practice generating differential diagnoses and care plans and exhibit the appropriate usage of x-rays and labs (PC,SBP,MK). A PGY 1 should evaluate no more than one to two new patients at a time. They should not accept responsibility for more patients until a senior staff member has evaluated his present patient. Their total caseload will be determined by their need for supervision, as well as patient acuity. PGY 2 and PGY 3 residents will be expected to further develop their clinical acumen, sharpen their physical exam techniques and hone their procedural skills. Their organizational abilities are expected to be more refined and they should be able to manage more patients simultaneously. PGY 4 residents are expected to “run the room” and act as junior attendings. They should know all the patients in the ED, facilitate their management and disposition, and supervise and teach junior residents and medical students.
At the completion of this rotation, residents should be able to demonstrate competency in and be able to:
- Decide which patients require admission, transfer, or discharge (MK,PC,SBP)
- Perform histories and physicals on Emergency Department patients (MK,PC)
- Understand the necessity for prioritizing patients (PC,SBP)
- Prioritize their activities (SBP,PC)
- Formulate differential diagnoses on their patients (PC,MK)
- Plan appropriate work-ups based on their differential diagnoses (PC,MK)
- Plan admission, transfer and discharges (PC,MK,SBP)
- Appropriately order and utilize laboratory data and ancillary studies (PC,SBP)
- Carefully understand and utilize universal precautions (MK,SBP)
- Appropriately utilize specialty consultation (P,C,PC)
- Function as a team member during resuscitations (P,C)
- Maintain patient follow up and rotation evaluation (PBL)
KCH Important Phone Numbers
| S-ED Areas | Paging | ||
| Suite A | 4616, 4617, 4618 | KCH | 3141, 3142 |
| Suite B | 4619, 4620, 4621 | Downstate | 718-270-2121 |
| CCT | 4601-04 |
||
| Fast Track |
4610 |
Overhead Paging |
*9 for waiting rooms |
| Peds |
3638,
3643, 3860 |
||
| Reception |
3183,
3185, 3187 |
||
| Triage - EMS | 1426 |
Zone paging |
dial *0, then… |
| Triage - Walk-In |
4638 |
Suite A |
24 |
| Suite B | 25 | ||
| Labs |
CCT |
26 | |
| Chemistry |
5342 |
FT | 27 |
| Hematology | 5373 |
Peds |
15 |
| Micro |
5354 |
Reception | 28 |
| Blood Gas |
4632 |
Rads Read |
13 |
| Blood Bank | 4897 |
||
| Offices |
|||
| Radiology | Dept. EM | 4790 | |
| CT
ED |
3378 / 1408 |
Fax |
4799 |
| S-2 |
3733 /
4985 |
Head RNs |
|
| XR Control | 4645 |
Medical Records |
4200 |
| MRI |
5585 |
Messenger |
4268 |
| Reading Rm |
1406, 1407 |
Patient Rep |
3917 |
| Ultrasound |
1405, 4699 |
Pharmacy |
7129 |
| Respiratory |
4526 | ||
| Inpatient Svcs |
Social work | 4628 (ED), 4011 | |
| Med RED Team | 347-231-5922 |
||
| Med BLUE Team | 347-231-5851 |
Environment of Care |
|
| Med Senior |
347-386-5976 |
Biomed (ECG, etc.) | 2932 |
| Peds GREEN |
917-760-0068 |
Facilities - daytime | 2943 |
| Peds RED < 4yo |
917-760-1301 |
off-hour |
2952 |
| electrical |
5138 | ||
| Behavioral Health |
plumbing |
2941 | |
| BH ER |
2310-12 |
IT Help Desk |
4357 (HELP) |
| BH - Internist |
347-992-7938 |
Linens |
4673 |
| Psy Consult - bpr |
917-760-0786 |
Telecom |
3333 |
| Office |
5209 |
||
| Units |
|||
| Outside #s |
CCU |
7580-2 | |
| FDNY Dispatch |
718-422-7395 |
Labor & Delivery |
4571 |
| FDNY Help Team |
347-865-8658 | MICU |
7583 |
| Medical Examiner |
212-447-2030 |
Morgue |
5313, 5423 |
| NYC Poison CC |
212-764-7667 |
OR | 4040 |
| PICU | 7028 | ||
| SICU |
7003 |

KCHC Main ED Junior Resident Clinical Role
The junior shifts at KCH offers a variety of unique learning experiences. The expectations of the junior residents at KCH are as follows:
- The junior resident is to follow each of their patients through to completion including initiating a workup, following diagnostic study results, obtaining appropriate consults, dispositioning the patient, and arranging appropriate follow up.
- If the attending picks up a patient primarily (which should be the exception and not the norm), the attending may ask you to perform any procedures for its educational value
- When the senior resident comes on shift, the junior may be assigned patients by the senior
- The residents are expected to precept medical students if there are no senior residents.
- As a benchmark, junior residents should try to see 1 patient per hour (PPH) in the main ED.
- As the junior resident you may be assigned to different areas of the Emergency Department by the RDOC.
- The junior resident is expected to maintain timely, thorough, and complete medical records in the T system and quadramed.
- If no senior resident is present in their quad, the junior resident should assist the attending in keeping track of the patients in their area.
- The junior residents should also watch the white board to ensure that all ESI 2 patients are seen and evaluated promptly.
KCH Senior Resident Clinical Role (Main ED)
The Senior Resident is responsible for overseeing overall patient flow, disposition, and patient management for Quads 1+2 or Quads 3+4 in the main ED. This includes both primarily seeing patients as well as supervising junior residents. The attendings assigned to Q1+2 or Q3+4 will provide overall supervision for their respective sides of the ED.
The KCH senior should assign cases to the junior residents based on level and complexity. The KCH senior will also see patients primarily.
- Expected to see at least 1.5 patients per hour
- Be aware of and direct care for all ESI 2 patients (may include assigning patient to junior resident)
- Expedite dispositions and help manage flow on their assigned quads
- When precepting junior residents, the senior is expected to write an ED Quicknote
- Provide guidance and feedback to junior residents
All residents are expected to maintain timely, thorough, and complete medical records in Quadramed and the paper T system. The supervising attending must verify all resident documentation.
Pre-attending Role
Location: Kings County Hospital Center Emergency Department
Resident levels: EM4 and EMIM4/5
Responsibilities in clinical area:
- The pre-attending will work under the direct supervision of an attending at all times.
- The pre-attending is responsible for maintaining patient care, safety, and overall flow for Q3 + Q4. They may assign patients to residents and see their own patients in order to fulfill this responsibility.
- Resident supervision: The pre-attending is responsible for overseeing the care provided by all residents and students assigned in Q3 + Q4. This includes taking presentations, helping formulate a plan of care, ensuring timely testing, treatment, and disposition, as well as writing a brief assessment and plan for all patients in which care was supervised.
- The pre-attending will be expected to direct rounds and assign sign-outs during change of shift for Q3 + Q4.
KCH PEDICATRIC EMERGENCY DEPARTMENT
- Administration
Dr. Konstantinos Agoritsas is the Director of the Division of Pediatric Emergency Medicine. Josepha Miranda is the Senior Associate Administrative Nursing Director for the Dept. of Emergency Medicine. Mrs. Loretta Lawrence Reid is our pediatric head nurse.
Pediatric EM, EM and pediatric faculty staff the Pediatric ED. Pediatric Emergency Medicine fellows, residents from the departments of EM, Pediatrics, Family Medicine and the combined EM/IM program rotate through the Pediatric ED. Third and 4th year medical students, as well as PA students also rotate through the Pediatric ED.
About 33,000 sick and injured children are seen in the Pediatric ED annually.
- Age criteria
Please use age limit criteria as guidelines and do not let patients suffer because patient is presenting in a “wrong ER with a wrong age”.
a) Medical emergencies <19 years of age = Ped ED
b) Minor blunt trauma <19 years of age = Ped ED
c) Major blunt or penetrating trauma up to 13 years of age = Ped ED
d) Major blunt or penetrating trauma after 13 years of age = Adult CCT
e) Surgical emergencies up to 18 years of age = Consult Pediatric surgery
f) Surgical emergencies in patients older than 18 years of age = Consult General Surgery
If a patient is followed regularly by one of our subspecialty clinics (e.g. asthma or sickle-cell clinic), we will see these patients up to their 21st birthday. If a discrepancy exists, the attending of record will make the ultimate decision as to where the patient is seen.
- Triage
When the patient first comes to the Peds ED, he/she is first evaluated by the visual triage nurse who will determine if the patient needs to be seen immediately or if stable, to be triaged and then seen by the physician . Simultaneously, the clerical staff will log in the patient to our registration system. The area clerk will complete full registration later. The triage nurse will then assign acuity of visit (ESI). Triage policies can be obtained from the Pediatric ED Nursing office and are available on the KCHC intranet.
All patients brought by EMS are triaged at the EMS receiving area. After triage, a physician can determine that the patient can wait in the waiting room, depending on ESI triage category, and conditions in the ED. Make sure the patient is triaged before the patient is asked to wait in the waiting room.
Patients presenting with acute asthma are seen by the triage nurse at the front desk or by the main EMS triage nurse and brought immediately to the asthma room for treatment. The nursing staff/ respiratory therapist assigned to the asthma room gives nebulization treatments.
- Patient care areas
- Rooms #1-5 are equipped with monitors, oxygen and suction and may be used by any patient.
- Room # 6 is generally used for fractures, procedural sedation and analgesia.
- Room # 7 is used for surgical procedures such as lacerations, I&D, etc..
- Room #8 has stirrups for gyn exams.
- Room #8 contains gyn supplies.
- Room #12 is an isolation room equipped with negative pressure and has its own bathroom and monitor. Any patient with exposure to measles, chickenpox or other infectious disease requiring isolation will be placed in the isolation room and evaluated there by the physician.
- Critical patients
If a patient is critically ill, they may be taken to the Pediatric CCT area or managed in one of the bays in pediatrics, usually Room 1, based on the attending’s preference and room availability. The charge nurse and the attending/PEM fellow are responsible for assigning the roles during the resuscitation. Please visit the CCT Pediatric Trauma Room and get to know where equipment and materials are located. A Pediatric Broselow cart is available in the CCT Pediatric Trauma Room and in Room #1 of the pediatric ED.
- Pregnant patients
Pregnant patients with a fetus of less than 20 weeks gestation are to be seen in the Pediatric ED.
Those presenting for something unrelated to pregnancy (eg- laceration/ tooth pain/ sprained ankle etc.), are to be cared for in the pediatric ED.
Patients with a fetus greater than 20 weeks gestation in active labor should be sent to Labor and Delivery Suite after initial triage and ED stabilization.
- Telephone triage
We do not give advice over the phone. Parents calling from home seeking advice are advised to seek treatment at the KCHC walk-in clinic, ED or their primary medical doctor. However, if the patient was seen within 72 hrs. and has a question related to the ED visit, you should answer their question and document “Other Contact” note in Quadramed EMR.
- Nursing
A charge Nurse is assigned 24 hours a day and is responsible for knowing the general status of the ED at all times. The charge nurse can help coordinate admissions, discharges and transfers. The nursing staff is comprised of clinical nurses, nursing support technicians and unit assistants. Each patient, once registered, is evaluated and a primary nurse is assigned. Emphasis is placed on collaborating with the nursing team for patient care and decision-making. This will definitely lead to a cordial work environment and the best patient care.
- Discharge instructions
Computerized Discharge Instructions and patient education materials can be printed out directly from the Micromedex R system and MD consult which are available through the computers at caregiver stations. The parent or patient must sign a copy of disposition note before being discharged. Statements like “preprinted discharge forms given to mother - she understands” shows that communication did occur.
It is very important that you document the following on all discharge instructions:
1) When to follow up: Many discharged patients require mandatory follow up. These include fractures, pregnancy, wound or burn care, or first urinary tract infections. Other patients do not warrant mandated follow up and thus the disease/illness will simply run its natural course. However, it is important to advise “as needed” follow up when it is appropriate to do so. If the condition improves as expected, no follow up is necessary. However, the instructions must clearly and specifically state that if the condition persists or worsens or some other problem develops, follow up is necessary.
2) With whom and where to follow up: Specify a date, time, and location and with which specialty the patient is to follow up. Depending on specific insurance issues, the patient may require a referral. Please advise the parent to seek additional assistance with their primary care provider regarding the referral process. If the patient requires immediate follow up at KCHC, an appointment can be made for less than 72 hrs, even if KCHC does not participate in the patients insurance. However, this should only be reserved for those patients who required immediate and definite follow up within 72 hrs.
3) Provide instructions in plain, simple language.
4) Avoid the use of medical abbreviations and medical lingo. Please write in a clear language that the patient or parent can understand. For example, instead of “q” write “every” and for ‘P.O.’ write “by mouth”.
5) Provide discharge instructions in the language of the speaking patient/parent.
6) Document that a translator was utilized when discharging a patient with the assistance of a translator. Always record the name of the translator on the discharge instructions or in the medical record of the ED visit.
7) Document a discharge diagnosis, even if it is an impression.
8) Provide specific instructions regarding home care for the patient’s injury or illness.
These instructions can range from brief instructions such as PRICE (Protect, Rest, Ice, Compression, Elevation) after an orthopedic injury to extensive information with computerized discharge instructions. When you provide a patient/parent with instructions from Micromedex R system or MD consult R, then document in the ED discharge instructions that the parent was provided with them. (Ex: Micromedex instructions on asthma in children given)
There are discharge instructions for several common pediatric illnesses on the clinicalmonster.com website. These instructions must be edited to fit the patient who is discharged home.
- Social work
• Social work can call ACS (Administration for Child Services). There is NO RULE that only physician can call ACS. Social work can also help in providing referral to community resources and agencies. Usually a 24-hour coverage and assessment is available for child abuse and neglect cases. If a social worker is not available (e.g. mid night-AM shift), please page AOD and they will get a social worker on the phone to assist / guide you.
Physical and sexual abuse
• Patients 18 years and younger fall under child protective services/specialist (CPS) laws and therefore, should have a pediatric consult. The Pediatric ED must ensure proper referrals to CPS, Social Services and appropriate counseling.
• There is a camera on a computer on wheels (COW) available in the Ped ED to document the signs of abuse. These photos must be uploaded into Quadramed. Please speak to the head nurse for assistance. You must document the name, MR# and who took the picture on each photo. Also, if you are documenting signs of physical abuse, place a ruler or another object (quarter) next to the physical finding in order to provide a perspective on the severity of the injury.
• From the ED, all patients who were evaluated for suspected or confirmed child neglect or abuse (physical, sexual) are required to follow up in the Child Advocacy Clinic, which is hosted by Dr Richard DiPasquales..
Child Advocacy Clinic
- This clinic is held every Monday, 9a-4pm and Thursday 9a-4pm in the E- Building 4th floor.
- Appointment MUST be made through the clerical staff of either Ped ED or registration
- Tel # of clinic: (718)-245-3612
Sexual Assault in Patients greater than 13yo
• Consult Sexual Assault Response Team through the page operator (# 3141). A general history and physical should be done, lab work drawn as per SART protocol. Social work should be consulted.
• These patients should be referred to adolescent medicine for follow up.
- If they receive medication for HIV prophylaxis, please be sure to tell them that although they receive medications/ prescriptions for 5 days, the entire course is 30 days.
- Consults
• Consults can be called via the page operator at #3141. If the operator states that the consult must be called through Downstate, please call 718-270-1212.
• All consult requests must be placed in the computer as an order.
• If the patient is to leave the ED for consults to dental, ophthalmology, ENT, Gyn, the chart will remain in the ED, and make sure that patient is sent with a nurse’s aide. Please make sure to provide all pertinent information in the EMR Quadramed.
• Please make sure that patient is not discharged directly by the sub specialist. You must co-ordinate discharge and follow-up with the consultant service.
- Psychiatry consultations
• There is child psychologist for consultation (Dr. Feldman) between 9 a.m.- 5 p.m., Monday-Friday. Instructions on how to contact psychiatry are in the Pediatric ED Resource binder and on SharePoint under Pediatric ED Resources. Between 5p and 9a and on the weekends/ holidays, the psychiatry on call individual will come to the PED to evaluate the patient, and if the patient requires admission, he/she will be transferred to R building inpatient unit after insurance clearance. If there is a delay in obtaining insurance clearance or if there are no available beds, the patient will be transferred to CPEP.
• All patients that are transferred to the R building need to be “medically cleared” and the psychiatry internist is to be informed, as well as the psychiatrist in the R building ED.
• Once the above communications have occurred, the patient may be transferred to R building with and aide and hospital police, along with a copy of the chart.
• If the child can go home, it is important that we refer them to the walk-in clinic in R building open M-F 9:00a.m. – 2:00 p.m.
• REMEMBER: Medical clearance in the Pediatric ED does not automatically mean routine blood tests like CBC and CMP. Patient can be medically cleared just by a history, and well-performed physical examination. Blood tests are ordered only when indicated.
- Admitting Process to Pediatrics
Inpatient Service
When you need to admit a patient to the pediatric inpatient unit, the chain of contact is as follows:
1) Page the resident at 917 760 1301.
2) If there is no response you can call the floor, but the first step is to page the resident.
3) If there is no response in 15 minutes, page the Pediatric Chief Resident at 9177600089.
4) Then the attending on call. The on call schedule for pediatric attendings is available in the Pediatric ED Resource Binder (blue binder).
5) Then Dr Chorny (Director, Pediatric Inpatient Unit)
6) Finally Dr Desai the Chief of Pediatrics.
PICU- All admissions to the PICU require a discussion between the PEM/EM attending in the Peds ED before the patient goes upstairs. The PICU resident can not accept the patient, unless the attending is aware. If you can not reach the PICU attending on call within 20 minutes and it is emergent, then you can reach out to the Director of the PICU, Dr Talaat Abdelmoneim at Cell # 646-533- 2599 and then to the Chief of Pediatrics, Dr Ninad Desai. (See Pediatric escalation policy on sharepoint). The resident in the Peds ED should then inform the PICU resident about the admission.
Other Important Notes about admissions
• Teens with gynecological issues, early (<14 weeks) pregnancy issues and or major medical problems needing pediatric care will be admitted to pediatric service on a pediatric unit and will be followed jointly by both services (Pediatric team as the primary and OB as consulting). In case of controversy, the responsible attending physicians will escalate the issues to Chiefs of Pediatrics and Obstetrics/Gynecology or their designee as appropriate. For any questions related to this: Page the Chief of Ob-Gyn via operator at 347-386-8360 Contact Dr Desai for Pediatrics- Beeper : 917-205-7317 or Dr. V. Chorny : at beeper 917-219-3591.
• All indicated diagnostic work-up, including labs, intravenous access, and first dose of antibiotics, (if indicated) are to be done in the ED. However, there are no routine lab tests that are required for admission (thus, a child getting admitted for Status Asthmaticus who is not dehydrated does not need BMP just because you are admitting him or you have extra blood drawn by a nursing staff).
• All the admissions to PICU need to be accompanied by a nurse and a physician. Physician-to-physician communication and nursing –to- nursing communication must be done in detail at the time of admission.
Remember: No one from the in-patient service or PICU has a right to refuse an admission (provided there is a bed available). Please page the AOD, and director of service (if required), if you have any difficulty admitting patients.
Admissions of status asthmaticus
GUIDELINES FOR MONITORING PATIENTS WHO WERE TREATED WITH INTRAVENOUS MAGNESIUM SULFATE
BACKGROUND: Intravenous Magnesium Sulfate is considered an adjunct therapy for patients with moderate to severe status asthmaticus and may be given to those who have had an inadequate response to first-line medications. Serious adverse reactions after a single dose of intravenous Magnesium Sulfate are rare, yet the potential for development of hypotension and arrhythmia warrants close cardiac monitoring during infusion.
At the time of the writing of this policy, there are no large clinical studies addressing the issue of optimal length of monitoring after Magnesium Sulfate infusion, and the following proposed guidelines are based on current clinical practice and knowledge about the pharmacologic properties of Magnesium Sulfate when given intravenously.
- All patients who have received intravenous Magnesium Sulfate should be placed on a cardiac monitor for ONE hour after completion of the dose. In most cases, this will be accomplished while the patient remains in the Emergency Room.
- Nursing report and physician hand-out need not be delayed until the end of the one hour observation period.
- Patients being admitted to the general pediatric ward before the required observation period has been completed should be placed in MONITORED BEDS. Patients deemed clinically stable for floor status may be moved from a monitored bed to a regular floor bed ONE hour after completion of the Magnesium Sulfate infusion.
- If monitored bed on the inpatient ward is not immediately available, patients should remain in the ED until one hour observation period is satisfied.
- In case no monitored bed is available, the floor team under attending guidance will review and assess the clinical status of the patients currently occupying monitored beds and make reasonable efforts to downgrade patients to regular floor status in order to accommodate a patient requiring close observation after Magnesium Sulfate. If the above is not possible, the floor team should discuss admission to the PICU for monitoring with the respective PICU team.
- If an agreement about a patient’s ultimate disposition cannot be reached between ED, inpatient and /or the PICU teams, the discussion should be escalated to the Directors of Service as per existing policy.
- In-patient wards
Pediatric In–patient ward is on D-6. (in-patient tower / “D” building 6th floor). PICU (8 beds) is located also on the D-6 North. There are also 4 observation beds (“stepped –down” unit) located on the D-6 north.
Neonatal ICU is located on D-5 (“D” building 5th floor) along with regular nursery.
- Transfers
- Outside ED to KCHC ED:
-Document pertinent information on ED Transfer/Referral Form located in the Transfer-Referral Binder.
-For all transfers requiring subspecialty care, you must confirm that the subspecialty accepts the patient prior to transfer. This includes urology, trauma, neurosurgery, orthopedics.
- Direct Admissions: Outside ED/Inpatient/PICU to KCHC Inpatient/PICU:
-Admissions to the PICU should be directed to the PICU Attending on-call.
(See Resource Binder for PICU Attending on-call schedule and pager #’s. Please do not give out direct cell phone #’s.)
-Admissions for transfer to the Pediatric Inpatient Service should be referred to 718-245-DOCS, or to the Chief Resident on-call (pager # 917-760-0089).
-Documentation on the ED Transfer/Referral Form should be performed for all referrals to KCHC.
-Direct transfers from other institutions do NOT routinely need to come through the ED. However, in select circumstances, the Inpatient or PICU Attending may request that the patient be brought through the ED for reassessment or stabilization. This must be discussed attending to attending.
-IF only a brief assessment is required, vital signs must be performed and Other Contact Note documented in the electronic medical record (patient should already be registered as a direct admission). If unable to document electronically, please document assessment on paper and attach note to patient’s chart.
*KCHC does not have a transport team and does not arrange transport; the transferring facility must arrange for transport on their own.
ED to ED transfers can only be accepted by the PED attending or Fellow. Please document information about the transfer in the blue “Transfer Book”. If a PEM fellow speaks with the referring hospital, the attending must be informed of the referral immediately.
- Follow-up
• Try to NOT schedule patients to return to ER for follow-ups. Appropriate ED follow ups are for complicated wound checks, and extenuating circumstances. If you do ask the patient to return to the Peds ED for follow up, ask them to return between 8-10am.
• Appointments for KCHC patients can be made by the clerical staff of Ped ED or by calling the clinic appointment desk at telephone # 245-3651.
• Depending on the insurance, the PCP may be the only one that can schedule/request sub-specialty follow-ups because they may need a referral paper (prior authorization) from the PCP. Thus, always refer the patient back to the PCP (e.g. a patient with chest pain who needs cardiology clinic follow-up for Holter –send such patient to PCP first who will in turn will make an appointment with cardiology).
• There is a schedule (time/day) of all the clinics with their telephone numbers posted in the ED.
- Follow-up Culture
• The cultures for that day will print out at approximately 4 am on the computer printer
• Please do not throw this away
• The 7am attending will assign someone to look up these culture reports.
• All patients with positive cultures should be called back whether they are being treated appropriately or not. Whether there is a change in management based on the culture results- a record should be made that the patient was contacted- or an attempt to contact them was made.
• Under the patient name please click on "documentation/notes" under the visit number that the culture was taken. Click on Recall Note and then the reason for the recall (Micro result). Click either in person or telephone- put down the person's name that you spoke with and it will go to "word" where you can put down further documentation like: antibiotics prescribed, the pharmacy where you called, or parent will pick up rx etc. If contact was made and the issue is resolved, mark as "resolved".
• If the phone numbers are not working- a telegram must be sent. If 2 attempts have been made to call the family and they have been unsuccessful, a telegram must be sent. If it is warranted that another attempt be made, after describing your attempt in the Recall note, mark it “needs follow up tomorrow”, and it will re-appear on the next day's culture list.
If you need a telegram sent- please ask the clerk to provide the telegram form, and send it for you. Document in the Recall note that the telegram is sent, and the issue can then be marked as “resolved”.
To make the above process as painless as possible, when seeing a patient and sending any culture off:
• You should confirm the phone number in the chart/computer is the correct one or enter it in the discharge note so it can be pulled up again in case the number in the registration is incorrect.
• If you send off PCR studies for Chlamydia or Gonorrhea in the ED and then treat the patient with oral antibiotics and a “shot”, you must document that the patient was treated in the ED. This will allow the follow up of the positive culture to be aware of what happened in the ED.
- Helpful hints
• If you get overwhelmed in the Ped ED (multiple injured or ill children), you can always call Adult ED and speak to the attending in charge. He /she can always send some help whenever possible (REMEMBER : This is one department and we always work a team—like wise if Adult ED is very busy and need any help, please send ED residents to help.)
• There is NO “SIGNING OUT AGAINST MEDICAL ADVICE” in Ped ED. Be an advocate for a child and always try to resolve the differences of opinion with parents in such a way that a child’s health does not suffer.
• Parents are not allowed to leave children of any age alone. We will try to relieve them, if possible.
• The computer generates all lab slips. Each specimen must be labeled and placed in individual bags. Almost all specimens can be sent to the lab via the pneumatic system.
• Procedure notes must be written for each procedure done. Always obtain consent prior to performing procedures (e.g. Procedural sedation). Always document Time Out when indicated.
• The physician performing the procedure is expected to discard the used items after the procedure.
• No patient can be discharged until the patient is presented to the Attending who will then complete the chart. Please ensure that all the residents/ medical students / PA students working with you are aware of these.
• Concerns for equipment failure, need of supplies, or facility issues (outlet not working, sink is clogged, etc) (if not emergent) should be conveyed to Mr. Jerome Love at Jerome.love@nychhc.org or the charge nurse as appropriate.
- IMPORTANT PEDIATRIC PHONE NUMBERS
Laboratory Emergency Medicine(4790)
Blood Bank 4897 4898 Admitting 7403
Blood Gas 4632 4633 Admin Front 3183 3185
Chemistry 5342 5579 Adult Reg/Triage 4637 4638
Hematology 5373 5348 Asthma ED 4611
Microbiology 5354 5355 CCT 4601
Parasitology 5364 EM Chiefs 917-761-1405
Serology 5364 Fast track 4610
Virology 5355 Labs/Delivery 4558 4571
Suite A/B 4616 4620
Radiology Pediatric Emergency Medicine
Peds Portable 4383 4382 Peds ED 3638 3636 3643 3861
Adult Portable 4645 Peds Pager 917-760-1301
Radiology Dpt 4380 3373 Peds floor(D6 N) 7023 7024
Cat Scan 4462 3378 Peds floor(D6 S) 7033/4 7042
Rad Resident 1406 1407 Peds Clinic 3652 2982
IR 4464 Peds Triage 3646
Nuclear 3696 Peds Floor 3612
MRI 2609 5585 Peds Chief 917-760-0089
Dr. Goldfisher 4453 pg.917-218-2968 PICU 7028 7029
Dr. Amodio 917-218-6321 NICU 7048/16/48/20
Ultrasound 1405/6 4690 or 917-218-5458 Child Psych inpt 2221/23/25
Rad Senior 917-760-1124
Other KCH Numbers
Housekeeping 4321 Area D 3651 3652
Laundry 2916 Cast Rm 5588
Linen 3977 4673 Clinic Appt 3325
Locksmith 3966 2156 Echo 4560
Maintenance 2952 2953 EEG 4714 4233
Plumbing 2941 Employee Health 3536
Escort 3994
Other Hospitals IT 8132
Bellevue Peds ED 212-562-3025 L&D 4571
Bellevue Adult ED 212-562-3015 Med Records 4200
Brookdale ED 718-240-5000 Med Examiner 212-447-2413
Cornell Burn Unit 212-746 5454 Messenger 4268
Jacobi Burn Unit 718-918-6066 MICU 7583
LIJ Transport 516-719-5437 Morgue 5423
Midwood Ambulance 718-645-1000 OB 4598 5443
Poison Control Center 212-POISONS Operator 2*#21
Ambulette 718-273-3555 OR 4094
SIUH Burn Unit 718-226-9000/1506 Psych ED/R Bldg 2312
UHB Operator 718-270-2121 Pharm D/B 7129 4313/16/19
Pharmacy(Kings) 718-363-3300
Other Important Contacts Psych on call 917-205-4735 or 760-1277
Mr. Jerome LOVE 5648 Rapid HIV 2410
Ms. Forte 4623 Respiratory 4526
ACS 1-800-635-1522 SART 3151
Dr. Dipasquale (Abuse) 917-879-4551 Security 4300
Sharps Change 5218
Dr. Agoritsas 347-672-9865 (cell) SICU 7003
3647 (office) Soc Work 4628 4374

Revised December 2012
- Extramural Deliveries
See Extramural policy available on sharepoint, but the general procedure is as follows:
(1) The Medical and Nursing staff of the CCT and the Pediatric ED (hence forward referred as “CCT team” for CCT physicians and nursing staff and “Pediatric team” for Pediatric ED physicians and pediatric nursing staff) will prepare for the extra mural birth.
(2) Emergency Department staff will notify Labor & Delivery at extension 4570 or 4571. If necessary, Neonatal ICU should also be called at extension 7048.
(3) On arrival in the ED, the mother and baby will be assessed by the ED physician, registered by the clerical staff and appropriately identified with a mother and baby ID band placed on both mother and baby (the baby will have the mother’s band in addition to the baby’s band and the mother will have the baby’s band and the mother’s band).
(4) After mother and baby are determined to be stable, both will be transported to Labor & Delivery by the CCT nursing staff where foot printing will be done.
(5) If the baby requires admission to Neonatal ICU, the pediatric ED nurse member who identified the mother and baby in the E.D will go to the unit to ID the baby to the Neonatal ICU staff to confirm baby, while the mother will be transferred to L&D. Foot printing will be done by the Neonatal ICU staff.
- Elevated Bilirubin Levels
Patients with elevated bilirubin levels who require phototherapy will be admitted to the NICU immediately after triage and evaluation by the peds ED physician. The patient can be admitted to the NICU and the additional work up (iv, repeat labs) and phototherapy will be started in the NICU. If the patient is sick and needs rescuscitation or fluids immediately, then initiate care in the peds ED. Patients with increased bilirubin levels from the clinic should be directly admitted to the NICU and do not have to come through the ED.
- Call back or radiology overreads: If you receive a phone call from radiology regarding an overread, you should document what you did in response to this information as a ED Recall note in QM. If you were not able to speak with the patient or family member, then enter the information in the ED Recall note, and document that the issue is NOT resolved. This issue will then print out on the ED Recall List which prints everyday in Fast track and Peds ED. An attending must be informed of the call back information and management decision.
- Documentation We are currently in a hybrid system where we use paper and electronic documentation. The plan is to document only in QM after July 1st. More information to come….
- Charts must be completed within 72 hrs, and preferably after your shift.
- Charts SHOULD NOT be removed from the clinical area. Do not take your charts home.
- Try your best to make sure the chart and the t sheet ends up together.
- Do not sign a t sheet that you would not feel comfortable defending.
- DO NOT SIGN AN INCOMPLETE t sheet thinking the resident will finish it later..
- If you have any charts that need to be submitted, dont hold on to them thinking they will go away. THEY WILL NOT. The charts stay on a report forever, so complete them and hand them in.
- Regarding documentation, make sure you document a EDQN on all patients you sign out who are admitted, transferred or still pending a workup. More to come on this.
- Groupwise Email accounts- All fellows and attendings who work at KCHC must have a groupwise email account. Please arrange with IT to obtain an account. If you have internet acces, then you have groupwise.
- Swaps in schedule (Attendings)
- Make sure swaps are made in tangier and reflected in tangier before the shift starts.
- Do not swap a shift and come back 8 hrs later (ex. come back at 7am after a 11p shift or come back at 6p after a 11p overnight), unless it is approved. You do not want this scheduled to you and unless it is an emergency it is not allowed by a NYS DOH law. it is also very difficult to leave at 11pm and come back at 7am
- Limit your swaps if the swap will not allow you to attend your non clinical responsibilities (committees, conferences)
- Do not swap if the swap leads you to work too many shifts that you would normally not want to be scheduled for.
- All swaps with a pediatrician who may work in the PEds ED must be approved by the PEM Director. In addition, the pediatricians can only swap into a 12-10pm shift (so a 11a-7pm shift). Again, these swaps must be approved and must be in tangier.
6) If you swap with a pediatricians who work a 10 hr shifts you will work 8 hrs likely 3p-11pm or 11-7 (depending on needs) and the pediatrician will work 10 hrs (12-10pm)
- Subspecialty services
- Pediatric Urology Physician Coverage- Currently there is no pediatric urology outpatient services at KCHC and at UHB. Both KCHC and UHB will have pediatric urologic emergencies covered by general urology. Do not refer to outpatient pediatric urology at SUNY Downstate until further information is provided. You should refer these patients to Bellevue Hospital for pediatric urology or to their pediatrician for referral to a pediatric urologist.
- Neurosurgery- There is no pediatric neurosurgery coverage at KCHC. Neurosurgery will evaluate all ED consults and make recommendations. However, patients who need pediatric neurosurgical management must be transferred.
- Orthopedics
- Orthopedic Cases that involve social work services: Any case that involves orthopedics and concern for child abuse/neglect will be admitted to orthopedics. Pediatrics will then complete a consult. Once the patient is cleared from orthopedics the patient will then be transferred to theg general pediatric service.
- Spica Casts for Femur fractures in the Peds ED: Spica casts will ideally be placed in the OR and not in the Peds ED. On the rare occurrence of the need for a spica cast, make sure that Dr Scott or the attending on call for Peds Ortho is aware.
- Transfers of Patients with Orthopedic Injuries from Outside Hospitals: Contact the Ortho attending on call before accepting transfers from an outside institution for orthopedic consultation/further management.
- Sign out and Rounds in the Peds ED
- Rounds must occur at change of shift at 7a/3p/11pm. You will be amazed how many times you will encounter patients that you thought you didn’t have, but you did something for.
- Rounds are a time for education..
- All patients MUST be signed out to an attending and a resident. This includes ADMITTED patients. An attending plus/minus a resident MUST know of the patient at all times. There is no such thing as patient is admitted so no sign out.
- Admitted patients in the Pediatric ED belong to us until they leave to go upstairs.
- Eating in the area is not acceptable. Please use the breakrooms to eat your meals. All beverages must be in closed containers with caps or lids.
- Front and Back Teams
- Last month we began to split the staffing into the front (1-6 and asthma) and back (rooms 7-12). The plan is as follows:
- Residents are split into teams as posted in the Peds ED, next to the “attending” computer.
- 7a, 3p, 11pm attending has the front rooms (when there are two attendings) or the entire Peds ED when there is only one attending.
- The 11a and 6p attending will come in and work the back rooms 7-12 plus assist the front attending with critically ill patients.
- The split teams must start at 7am with residents. When the second attending comes in at 11a or 3p their primary goal is to take the back rooms plus help out.
- It is best if the second attending and the resident/s in the back use the computers in the back. Both computers outside of room 8 print to the separate printer in the back as well.
- Ideally the back attending can assist in moving patients and knowing what is going on (who is at xray, who can step out of a room and wait in a chair or the waiting room, etc) and thus move patients along.
- It is not a perfect system, but if we continue to try and work in teams with the residents/pcas/RNs, communication will improve and thus patient care will improve as well.
- This does not mean that the attendings do not help each other out, but are encouraged to help. However, there is no reason that a patient is in a room and no attending knows about the patient at sign out, since if there are two attendings, each has their primary responsibilities.
- When the fellow comes in at 1pm, the fellow will assist primarily with the front rooms, but will also help precept all patients as needed.
- When a pediatrician is the second attending, the front PEM or EM attending has the entire ED, and the pediatrician will evaluate ESI 4,5s on their own or precepting pediatric residents. When there are two EM or PEM attendings, the pediatrician will utilize the Pediatric Fast track room next to pediatric triage.
- Escalation Policy for the Peds ED Stepwise Approach
Konstantinos Gus Agoritsas
- 3476729865 (work cell)
- 9179236600 (personal cell)
- If the above don’t work and is urgent, you can text and email (Email preferred) Service in the hospital is not great, so phone calls may not go through, but texts or emails work better somehow.
- Home # is 7182252745
- If you still haven’t reached me, then contact Dr Legome for clinical issues and Dr Karen Stavile for scheduling issues
- DO NOT LEAVE A MESSAGE ONLY IF THE ISSUE IS URGENT. KEEP TRYING TO CONTACT ME OR CALL DR LEGOME, DR JACKSON, OR DR STAVILE.
- Pediatric ED Resource Binder on Sharepoint
The following documents are available now and more to come:

- Pathways
Pain
Upon identification of a patient that meets the criteria for administration of medication for fever or pain at triage, the following standard has been developed:
1) The RN will call 718-319-6624 (Fellow/Senior Resident Phone, which will be kept in the charging station and any physician can answer and place the order in QM) THE BAT PHONE
2) Provide the physician the following information:
a. Name
b. MR#
c. Medication/Dosage
d. Reason for medication (fever or pain)
e. Allergies (if not in EMR yet)
3) Physician will then enter order in QM.
The above eliminates the waste in nurses walking back and forth to obtain a medication order and the interruptions for physicians who must stop to enter the order in the middle of another important task. If you have any suggestions on how to improve this process, please let us know.
Ultrasound for Pyloric Stenosis
An Ultrasound for possible pyloric stenosis is rarely an emergent study that must be done afterhours. Thus the following pathway has been agreed upon by pediatrics and pediatric radiology.
Scenario A) If patient is dehydrated/ requiring iv fluids/ there is concern for loss to follow up/ there is any reason for admission, please place IV, obtain CBC and chemistries, give IVF and admit for ultrasound in the morning. (The ultrasound for HPS is NON-URGENT)
Scenario B) In the well hydrated, well appearing infant with suspicion for pyloric stenosis- not requiring admission for other reason. (Primary differential dx is reflux)
At KCHC: Order limited ultrasound for hypertrophic pyloric stenosis - "scheduled"
At UHB: In FOX order: modality- "sono"; urgency- "tomorrow/ routine"; study- "abdomen limited"; working diagnosis- "pylorospasm"
On discharge please write detailed note something like "The baby may have something called pyloric stenosis (a narrowing of the exit of the stomach) to check if this is what he/she has, an ultrasound needs to be done. Please go to (S building for KCHC) 2nd floor Radiology and bring this paper tomorrow morning at 9:00 am to get the ultrasound done. If the ultrasound is normal, the baby most likely has normal baby reflux (spit-ups) but we still need you to follow up with your pediatrician in the next 1-2 days to be re-checked. If the ultrasound is abnormal (there is something wrong), you will be instructed to go back to the Emergency Department to be registered and treated."
At KCHC: Also, create an ED recall note under x-ray so that we have a way to make sure the patient went to radiology; please include patient phone numbers and any pertinent information and the message "please call on XX/XX/XX to make sure they went to radiology for pyloric ultrasound".
At UHB: Place a sticker and contact numbers in the recall book with any pertinent information and "please call on XX/XX/XX to make sure they went to radiology for pyloric ultrasound".
This pathway can be found in the Pediatric Resource Binder in under P for Pyloric at KCHC and in the Peds ED Policy and Health Advisory and On Call Book at UHB.
Fever in Less than 21 days- Bottom Line: 1) must have CSF herpes PCR collected 2) acyclovir should be started in the Pediatric ED if those conditions highlighted in green are present

KCHC Pediatric ED Resident Clinical Role
The shifts at KCH offers a variety of unique learning experiences. The expectations of the junior residents at KCH peds are as follows:
- The resident is to follow each of their patients through to completion including initiating a workup, following diagnostic study results, obtaining appropriate consults, dispositioning the patient, and arranging appropriate follow up.
- The resident is expected that they meet EMS as they bring patients into the ED.
- The residents are expected to be present at all notifications and pediatric resuscitations.
- If the attending picks up a patient primarily (which should be the exception and not the norm), the attending may ask you to perform any procedures for its educational value
- When the senior resident comes on shift, the junior may be assigned patients by the senior
- The residents are expected to precept medical students if there are no senior residents.
- As a benchmark, junior residents should try to see 1.5 patient per hour (PPH) and 2.0 pph for seniors in the main ED.
- As the resident you may be assigned to different areas of the Emergency Department by the RDOC.
- The resident is expected to maintain timely, thorough, and complete medical records in the T system and quadramed.
- The residents should also watch the white board to ensure that all ESI 1 and 2 patients are seen and evaluated promptly.
UHB EMERGENCY SERVICES
Introduction
The purpose of this orientation manual is to orient you to the UHB Emergency Services and to help you prepare for your rotation through our department. It is assumed that by this time you have received your clinical shift schedule and spoken with/met with Dr. Foley or Dr. Mehta, as well as the Chief resident to prepare for the rotation. You will receive a tour of the facility highlighting the physical plant and a description of the available resources and supplies (including airway medications and supplies, resuscitation carts, etc.). In addition, you are expected to be familiar with the UHBES Policy and Procedure Manual, a copy of which can be found on the unit or in the Medical Director’s office.
The University Hospital of Brooklyn
UHB is a 400-bed tertiary care hospital located in the Flatbush section of Brooklyn, New York. The hospital is affiliated with SUNY--Downstate Medical School, with a graduating medical school class of 200 physicians/year. The hospital’s capabilities include all surgical sub-specialties, dialysis, cardiac catheterization, OB/GYN, NICU, and transplant surgery.
Description of Unit
UHBES is a comprehensive Emergency Department . Our physical plant has expanded to a 9,000 square-foot unit with dedicated pediatric, adult and fast track areas. The annual census of the department is approximately 67,000 patients generating greater than 13,000 admissions to the inpatient wards. The unit is a FDNY EMS-designated 911 receiving center and is able to accept both BLS and ACLS ambulances from both the FDNY and private ambulance companies.
Roles and Responsibilities of Resident Physicians
The role of the Resident Physician in the ED is to provide excellent, timely and courteous medical care to our patients. In return, the resident can expect to experience fast-paced Emergency Medicine with a focus on quality medical care. The resident will encounter a “community-type” setting amidst a tertiary care atmosphere. Residents are expected to discuss all patient interactions with a faculty attending physician, and all medical decision-making must be initiated in concert with the attending’s supervision.
Patient Flow
All patients who present to UHBES will be triaged based on severity of illness and receive an appropriate medical screening exam for their stated medical complaint. It is the policy of UHBES that all patients are to be triaged within fifteen minutes of presentation. Financial information may be obtained during the medical screening process but may not impede the completion of the medical screening exam. All patients will receive a medical screening exam to determine if an emergency medical condition exists. Patients who are determined to have an emergency medical condition will be stabilized utilizing the full resources of the institution irrespective of the patient’s ability to pay. After notification of the inpatient service the attending physician may admit patients who require admission. You must discuss all admissions with the faculty attending physician prior to initiating the admission process. Patients who require services not provided at UHB will be offered transfer to an appropriate facility.
Consults
Specialty consultations are available in all services offered by UHB. The consult policy mandates that all emergency consultations be answered by phone within 10 minutes and in person within 30 minutes. It is expected that the physician requesting the consult will complete and sign the required green consultation form (UHB 44). Urgent consults may be seen within 3 hours. If, as the resident physician, you are having difficulty contacting a given service, you are to discuss this immediately with the ED faculty attending of record for the case. Obstetric consultation for all stable pregnant patients will take place in the Labor and Delivery unit (NS 33)—you do not need to inform the OB service prior to sending stable pregnant patients upstairs. However, you must discuss the status of the patient and the faculty attending must examine the patient prior to the patient leaving the unit. The details of the consultation policy may be found in the UHBES Policy and Procedure Manual. Patients may only be sent to outpatient suites [dental, ENT, GYN (suite G)] for emergent consultations at the discretion of the attending physician, and only if accompanied by qualified medical personnel. In addition, patients should not be sent for follow-up care at outside institutions (i.e. KCHC, etc.).
Admitting Process
At the time it is determined that a patient requires admission to the hospital, you must discuss the case with a faculty attending physician. EVERY admission needs to be endorsed to the appropriate accepting service. The endorsement process starts with electronic text paging via our “access admit log” which is on the desktop of most of our PCs. You will be given a user name and password at the beginning of your rotation. Upon inputting the name and diagnosis of the pt, an automatic page will be placed to the correct resident on call who will call back for a report. This will also create a permanent record of the page. Patients without an attending physician at UHB are to be admitted to the attending-on-call for the required service. Residents may act as proxy to accept admissions but may not refuse admissions. All admissions must be discussed, either in person or by phone, with the admitting attending of record or his/her proxy. No patient is to be admitted to any service without prior appropriate notification. Monthly call schedules for all UHB services are to be found in the blue on-call book. The details of the admissions policy may be found in the UHBES Policy and Procedure Manual. The resident should document in the medical record with whom the case was discussed (Private Attending, On-call house-staff, consults, etc.) and at what time this occurred. The Department of Medicine has in place a hospitalist program to provide medical coverage for patients who are to be admitted who do not have a personal physician.
Progressive care unit: Patients with new onset CHF, exacerbation of CHF, new onset a.fib, NSTEMI, arrhythmias, etc. should be seen by cardiology for evaluation and admission to PCU. Please refer to the admission criteria posted in the ED.
Boarders
Patients who are admitted to the hospital but who do not have beds are to be cared for by the admitting service. The transition to the in-patient team takes place at the time admitting is called and the team notified, NOT at the time a bed is assigned. The inpatient team is expected to write admitting orders and provide care. The ED attending is expected to intervene if any emergency arises or the patient’s status changes. The details of the boarder’s policy are in the UHBES Policy and Procedure Manual.
ICU Admissions
The respective unit must accept patients who require admission to either the MICU or CCU. If a dispute arises about the ICU admission the discussion must be attending-to-attending and all involved services must be part of the discussion. Currently there is an intensivist in-house 24-hours daily. If the ICU cannot take the patient because of operating above capacity, the ICU team may accept the patient as a boarder and care for the patient in the ED. If the ICU will not care for the patient the director of the ICU, the administrator on duty, and UHBES Medical Director are to be notified.
UHB Admitting Process
There is a number of inpatient admitting services at UHB that each has a process for accepting ED admissions.
Family Practice:
The FP service cares for its clinic and private patients when they are admitted. For patients that are followed in Suite B (resident and attending clinic) and Lefferts Ave Family Health Services, call the FP resident on call. If necessary, you can page the patient’s attending physician as well but this is not always necessary. When you have identified a patient of theirs that will likely require admission, start the process early as they may want some consults before taking the patient on their service.
Medicine:
The Internal Medicine department has three possible admission pathways:
- Private patient-PA Service: There are five PA teams that cover a number of private Downstate MD’s. The list is located above the computer in the physician area of nursing station A. While you don’t need to memorize the teams, you need to recognize the names of the private MDs that admit via the PA service. You must speak with the physician as the PAs cannot accept an admission on behalf of the attending. After discussing the patient with the PMD and admission is agreed upon, a brief call to the PA team is strongly recommended especially on ‘off hours’ to endorse the patient but is not required. Patients that have a PMD through Preferred Health Partners (PHP), are admitted to the PHP hospitalist group.
- Hospitalist service-Medicine admitting resident: Patients that do not have a primary care MD with admitting privileges to UHB but require inpatient care are cared for by the Hospitalist service. The UHB Hospitalist group admissions go through the Medicine admitting Resident. There is a text page system ‘ERMED’, which requires a user ID/Password that alerts the admitting medical resident to patients that require admission to the hospitalist service. The case is then endorsed to the medical admitting resident who accepts the case on behalf of the attending.
- Private patients-medicine resident: There are a few private MDs that do not use the PA service. These admissions go through the same ERMED text paging service.
Subspecialty Services:
Cardiology has two inpatient services
- Progressive Care Unit: Inpatient cardiology service that can manage CHF exacerbations, rapid afib, non-critical NSTEMIs, high-risk chest pain patients, etc. There is a fellow assigned to this service as well during the day and the on-call cardiology fellow during off hours.
- CCU: inpatient cardiac intensive care unit that has a cardiology fellow assigned during the day and the on-call cardiology fellow on off hours.
Renal Service:
- The renal service accepts admissions for patients that require inpatient care who receive their dialysis at Parkside, the Downstate Ambulatory Dialysis Center. These admissions go through the Renal Fellow who will endorse the case to the MAR.
Neurology:
- There is a neurology inpatient service that accepts admissions for neurologic diseases through the on-call neurology resident.
- The Stroke Unit is the neurology step down service that accepts admissions for Stroke patients and neurology patients that require monitoring.
- Seizure – There is seizure inpatient service who will accept admissions with this diagnosis who are their patients or do not have a physician at downstate. The seizure service is different the neurology, however, the neurology service will often be aware of the best manner to contact the seizure service.
Surgery:
General and all the surgical subspecialties require consultation prior to admission.
There is an in-house Surgical Hospitalist attending available 24/7 for all consults/admissions.
Orthopedics:
1. The orthopedic service can and should admit appropriate patients. There is an agreement between the ED, Ortho, and Medicine departments regarding pts with significant co-morbidities that will require orthopedic inpatient care. If the ortho service is uncomfortable with a pt with uncontrolled medical issues, they can request a Medicine consult. If it is determined by Medicine and the ED attending that the patient is stable for ortho admission, they are admitted to Orthopedics. If the patient has uncontrolled medical problems with a concurrent orthopedic condition, they can be admitted to medicine with orthopedics as a consult service.
Transfer Agreements
Transfer agreements are in place and protocols approved for the following inter-facility transfers once initial stabilization has been achieved:
Burn: Patients requiring burn unit admission are to be transferred to NY Hospital, Cornell University or Staten Island University Hospital.
Hyperbarics: Patients requiring hyperbaric therapy are to be transferred to Jacobi Hospital.
Trauma/Pediatric Psychiatry: Patients requiring admission to either of these services are to be transferred to King’s County Hospital Center.
Neurosurgery: All Neurosurgical patients are to be transferred to UHB-LICH
All transfers must be discussed with an accepting physician at the receiving institution, and prior to transfer, all patients must have a transfer form (UHB #7-83) completed by the Attending Physician, including reason for transfer and the name of the accepting physician at the receiving institution. In addition, the UHB AOD is to be notified prior to transfer.
Pediatrics
Pediatric patients comprise approximately 30% of the UHBES patient census, and as such will comprise a significant portion of your clinical duties. Our facilities provide a dedicated pediatric ED, including full-time pediatric triage, nursing and physician and physician-extender coverage under the direction of Dr. Nooruddin Tejani, Director of Pediatric Emergency Services. During periods when there is not a dedicated pediatric attending or pediatric resident, you will be expected to care for pediatric patients. Pediatric admissions (NS 42) are to be discussed with the pediatric resident on-call, who can be contacted by calling the pediatric unit. Any child who you feel requires ICU or step-down monitoring must be discussed with the pediatric attending intensivist (NOT the Chief Resident). A large segment of our pediatric population is primarily cared for by Downstate Pediatric Associates (718-998-5076) who request that they be notified of all patients affiliated with their group who present to the ED for care. The pediatric ED also keeps a log of all cultures that are taken on a daily basis. The residents will be expected to help follow up the culture results and call back patients as needed.
UHB Administration
- John Williams, MD President, SUNY Downstate Medical Center
- Ian Taylor, MD Dean, SUNY Downstate Medical Center
- Michael Lucchesi, MD Chairman, Emergency Medicine,
Chief Medical Officer – SUNY Downstate
- Roger Holt, MD Vice Chair - Emergency Services
- Mathew Foley, MD Medical Director Emergency Department
- Ninfa Mehta, MD Assistant Medical Director Emergency Dept
- Nooruuddin Tejani, MD Director of Pediatric Emergency Services
- Judy Drummer, RN Assoc Director of Nursing, ED
- Vikki Small Administrator of Emergency Services
Ancillary Staff
Ancillary services in UHBES are provided by the EKG technicians and Healthcare Assistants (HCA I and II). The EKG technicians’ responsibilities include phlebotomy (but not intravenous access), performing EKG’s, patient transport and clerk relief. The HCA’s responsibilities include patient transport, lab delivery, and patient care assistance. As a Resident Physician, it is expected that your time here will be spent on direct patient care, rather than ancillary duties. All IV access is to be obtained by either the RN or the MD. Techs and HCA’s can NOT obtain IV access. In addition, there is a dedicated ED phlebotomist in the ED from Noon-8p on weekdays.
Information Systems
At present, UHBES employs several information technologies. We utilize the electronic T-System (T-EV) as our EDIS, as well as our CPOS. You are expected to complete your training online via a link that will be emailed to you prior to starting your rotation. Please make sure you have all of your required passwords and training done PRIOR to your rotation at UHB.
Please see Dr. Foley or Dr. Mehta if you have any questions about the use of this system. The CERNER system is for lab entry and retrieval, and RIS for radiological procedure entry and retrieval. Prior to your starting in the ED, you should obtain your IS in-service. For RIS, see Mike Vaughn (x4613). It is absolutely imperative that you NOT share your login or passwords with your fellow residents, as this is a serious breech of hospital and departmental policy. If you need to renew or reset your password, please see Dr. Foley, Dr. Mehta or Ms. Vikki Small.
Nursing
The UHBES nursing staff is composed of one charge nurse, two triage nurses and at least eight RN’s per tour. UHBES nurses are all BLS/ACLS/PALS certified, and as such are qualified to provide care for Emergency Department patients. Intravenous access is to be obtained by the nurse assigned to that patient. Please be diligent in actively involving the nursing staff in your on-going management decisions regarding patient care. Many of the newly hired staff are young and eager to learn, but may need guidance in Emergency Medicine patient management.
Radiology Services
The Department of Radiology has made a commitment to our department to provide efficient, full-service radiology services. “Wet readings” of films may be obtained by paging the radiology resident on call during off hours or calling the radiology department during the day. We currently have an ED radiologist present in the reading room by CT. All plain films are to be reviewed by yourself and the attending physician of record on the PACS system, located in the ED. The senior radiology resident on call should be contacted to discuss all off-hour specialty studies, and the page operator should be utilized to page the technician. If there is difficulty contacting the technician, the AOD is to be notified and the radiology administrator is to be paged. Any persistent difficulties in obtaining studies should be referred to the attending radiologist on-call. All radiological studies are available 24 hours a day, 7 days a week, 365 days a year.
Laboratory Services
Lab studies are available 24-hours daily. It is your responsibility to discuss all lab test results with the faculty attending of record prior to disposition of the patient. Whole blood analysis for blood gases, chemistries, metHb and COHb are presently available on a STAT basis (turnaround time in minutes) 24 hours daily.
- Of note--BNP is available (must be sent in a separate lavender tube).
- ELISA D-dimer is also available for r/o PE/DVT, but MUST be utilized in conjunction with a pre-test Well’s criteria documented in your medical record.
Physician Documentation
All patients who present to UHBES are required to register and undergo triage, at which time a chart will be generated. Currently, we utilize the electronic T-system charting tool. It is expected that you will complete the patient chart, providing all pertinent historical, physical, and laboratory/radiological/EKG interpretive information—both positive and negative—prior to patient disposition. All patients must be discussed with a faculty attending physician. It is your responsibility to note on the chart which attending was involved in your supervision of the care of this patient (i.e. “d/w Dr. X”, etc.). If a patient is to be discharged, all patients must have specific discharge instructions (“exit-writer”), including time and place, return instructions, and any medication/care instructions. All charts must be locked by the end of your shift or no later than 24 hours after seeing the patient.
CPOS: computerized physician order system. We currently input our orders for medications, labs, and any ancillary tasks electronically in T-system. Radiologic studies, however, will need to be put in a separate system called RIS (the FOX). We hope to incorporate a fully integrated CPOE encompassing all radiologic and laboratory tests in the coming months.
Protocols
Code H: We have a STEMI pathway (called “code H”) that is to be initiated IMMEDIATELY upon presentation of any patient with a STEMI. Initiation of the cascade is to be signaled upon notification by FDNY EMS that a patient is en route with a suspected STEMI. The pathway is posted in the ED (outside the resuscitation room). Please make sure that the attending is involved immediately in any STEMI case.
Code S: This is the pathway for stroke patients. Initiation of the cascade is to be signaled upon notification by FDNY EMS that a patient is en route with a suspected CVA within the 3-hour window AS WELL AS the 3-4.5 hour extended window.
For both situations, please DO NOT call the operator yourself. Please ask one of our clerical staff as they are required to complete a logbook with the sequence of events and the times they occur.
Scheduling
ALL SCHEDULE REQUESTS ARE DUE AT LEAST FOUR (4) WEEKS PRIOR TO YOUR STARTING DATE. This is to ensure timely completion of your schedule and maximum clinical benefit from your rotation. All schedule requests should be emailed to uhbchief@yahoo.com. No written or verbal requests will be honored. You will be assigned a number of clinical shifts (usually ten hours in length, 8 hours for overnight) in accordance with your clinical requirements as dictated by the Department of Emergency Medicine. (Please note any religious commitments well in advance when making your schedule requests).
Of course, you are expected to be on time (10 minutes early) and to stay in the clinical area at all times. You must stay in the clinical area until your relief has arrived to ensure appropriate patient “sign-out”. The Director or Assistant Director of UHBES must approve all scheduling changes and “covered shifts” in advance. In addition, in the case of a personal emergency or illness, you MUST contact Dr. Foley or Dr. Mehta, as soon as you know you will not be able to attend your shift. You must also contact Ms. Stephanie Lane, the Chief Resident on-call and the Residency Director, Dr. Rinnert. All missed shifts will be made up.
Dress Code
As a representative of UHBES, it is expected that you will dress professionally in the clinical area. As such, “scrubs” are not permitted during daytime shifts (but are permitted on overnights).
PMD Notification
UHBES is committed to fostering a close, professional, and efficient relationship with the primary care physicians in our community. In an effort to enhance this partnership, you are asked to be diligent in your effort to discuss your care and disposition plans of all patients with known PMD’s who present to the ED. This includes both admissions and discharges. Please document on the medical record the name and time of the attending with whom you discussed the case. Please pay particular attention to the patients who are followed by the Family Practice service. They do have an inpatient service at UHB, and are almost always willing to accept admissions for their patients. The FP outpatient service is located in Suite B.
Ground Floor Response
In accordance with the EMTALA regulations, UHBES has accepted the responsibility to respond to all calls for assistance originating from the basement, ground floor of the hospital/medical school, and within a 250-yard perimeter of hospital/medical school grounds, including the Primary Care Annex. The attending physician is expected to provide medical coverage for these calls in conjunction with the “code team” response unit. This policy is outlined in the UHBES Policy and Procedure Manual. You may be asked to accompany the attending physician on one of these calls during your rotation.
Resources
UHBES is dedicated to providing the resident physician with the most up-to-date, clinically relevant Emergency Medicine resources available. To that end, internet access is available in the clinical area to allow you to research current guidelines in diagnostics and therapeutics.
Summary
In summary, we welcome you to our ED and look forward to working with you to develop your clinical skills and to facilitate patient care in our ED. We feel that our facility will provide you a unique Emergency Medicine experience, combining a community atmosphere with a tertiary care setting. Please remember that we are very open to suggestions on ways to improve our rotation—we want to work with you. Your feedback is very important to the success of your rotation, especially if you discuss your concerns in real-time--please do not wait until the end of your rotation to voice a concern or raise a suggestion. Again, welcome to UHBES.
Useful Phone Numbers
Roger Holt, MD Bpr: (917) 760-1994
Email: roger.holt@downstate.edu
Mathew Foley, MD Phone: (718) 270-8296
Phone: (718) 270-4442
Cell: (718) 300-5774
Email: Mathew.Foley@downstate.edu
Nooruddin Tejani, MD Bpr: (917) 760-0800
Email: nooruddin.tejani@downstate.edu
Ninfa Mehta, MD Bpr: (718) 270-4442
Email: Ninfa.Mehta@downstate.edu
UHB Chief Resident
Email: uhbchief@yahoo.com
Ms. Vikki Small ofc: x1586
Email: vikki.small@downstate.edu
Aquila Lewis ofc: x4442
Page Operator x2121
UHB Junior Resident Clinical Role
The junior shifts at UHB offer a variety of unique learning experiences. The expectations of the junior residents at UHB are as follows:
- When the junior resident is the sole resident in the main ED, it is expected that they meet EMS as they bring patients into the ED.
- The juniors are expected to be present at all notifications and medical resuscitations when they are the sole resident provider.
- The junior resident is to follow each of their patients through to completion including initiating a workup, following diagnostic study results, obtaining appropriate consults, dispositioning the patient, and arranging appropriate follow up.
- If the attending picks up a patient primarily (which should be the exception and not the norm), the attending may ask you to perform any procedures for its educational value
- When the senior resident comes on shift, the junior may be assigned patients by the senior
- The residents are expected to precept medical students if there are no senior residents.
- As a benchmark, junior residents should try to see 1 patient per hour (PPH) in the main ED, 1.5 PPH in the Peds ED, or 1.5 PPH in the Fast Track.
- As the junior resident on overnight shift you may be assigned to different areas of the Emergency Department by the attending.
- The junior resident is expected to maintain timely, thorough, and complete medical records in the T system. All charts are to be locked within 48 hours without exception.
UHB Senior Resident Clinical Role
The Senior Resident is responsible for overseeing overall patient flow, disposition, and patient management in the main ED. This includes both primarily seeing patients as well as supervising junior residents. When multiple senior residents are present, there will be a Resident-in-charge (RIC) designated who will precept intern cases as well as supervise procedures.
The RIC should assign cases to the residents based on level and complexity. The RIC will also see primary patients.
- Expected to see at least 1.5 patients per hour in the main area
- Be aware of and direct all resuscitations
- Expedite dispositions and help manage flow through the main ED
- When precepting junior residents, writing a progress notes and assessments on sick patients is expected
- Provide guidance and feedback to junior residents
When there are two senior residents, the non-RIC will see patients primarily and work on speed and efficiency skills.
All residents are expected to maintain timely, thorough, and complete medical records in the T system. All charts are to be locked within 48 hours without exception.
UHB “Resident in Charge” Clinical Role
This Senior resident will manage the emergency department. The purpose of the RIC is:
- To help our residents become better managers of a busy ED.
- To become comfortable simultaneously directing patient care while assuring that all resources in the ED are properly allocated.
- To become better educators and evaluators of junior practitioners through direct supervision of their patient care.
- To develop leadership skills while helping ED flow working with nursing, physician and support staff.
The responsibilities of the RIC are:
- RIC will evaluate every pt assigned to the main area of ED at triage.
- RIC will make an initial assessment of each patient that is brought to the ED and assign these patients to either themselves or another resident.
- RIC will facilitate ED flow by keeping clear and open communication with nursing leadership on the patient plans.
- RIC will keep an overall sense of the ED patient plans.
- RIC will triage radiological interventions, consultations and dispositions according to pt acuity, ED staffing and LOS.
EDUCATIONAL OBJECTIVES
EDUCATIONAL OBJECTIVES – PGY 1
- Emphasis during this year will be placed on orientation to the different emergency department environments. By the end of the year, the resident will demonstrate the ability to prioritize and organize activities; chart documentation; perform basic procedural skills; work with hospital staff; deal with friends and families of patients (particularly those who are critically ill or dying); and most importantly, perform quality patient evaluations. The resident should demonstrate accurate and appropriate history and physical exam skills; how to generate differential diagnoses and care plans; and the appropriate usage of x-rays and lab exams. A PGY-1 should evaluate no more than one or two new patients at a time. They should not accept responsibility for more patients until he or she presents the patient to a senior resident or attending. Their total caseload will be determined by their need for supervision, as well as patient acuity. The PGY-1 should expect their evaluation to be repeated by their supervisor. A PGY-1 cannot make independent admission, transfer or discharge decisions, but they should formulate and offer their plan for the aforementioned. A faculty member must co-sign all charts.
At the completion of this training year, the resident will demonstrate competence in and be able to:
- perform histories and physicals on Emergency Department Patients: adults and children
- understand the necessity for prioritizing patients
- prioritize their activities
- formulate differential diagnoses on their patients
- plan appropriate work-ups based on their differential diagnoses
- plan admission, transfer and discharges
- appropriately order and utilize laboratory data and ancillary studies
- carefully understand and utilize universal precautions
- appropriately utilize specialty consultation
- function as a team member during resuscitations
Description of clinical experiences:
First Year Residents should have experience and demonstrate competence in the following procedures:
- physical examination
- oxygen administration
- bag-valve mask device usage
- closed chest compression
- oropharyngeal and nasopharyngeal airways
- pelvic examination
- phlebotomy
- peripheral intravenous lines
- Foley catheter placement
- arterial blood gas sampling
- nasogastric tube placement
- thoracentesis
- vaginal deliveries
- central line placement
- lumbar puncture
- arthrocentesis
- paracentesis
- basic wound management
- incision and drainage of simple abscesses
- basic suturing of uncomplicated (non-facial, non-hand) lacerations
- splinting of strains and sprains
- anterior and posterior nasal packing
Core Competencies
Patient care
- Procedural practice
- Physical exam
- Formulate treatment and disposition plans
- Triage of patients and prioritization
- Practice experience
- Skills labs
- Simulator time
- SDOT
Medical Knowledge
- Conference attendance and participation
- Topic review groups
- Webtests
- Inservice exam
- Bedside teaching rounds
- Responsibility for preparing case conferences
- Participation is skills labs
- Simulator time
- SDOT
Professionalism & Interpersonal
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Responsibility for presenting case conferences
Communication
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
System based practice
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Participation in CQI committee
- Participation in M&M committee
Practice based learning
- Simulator time
- Participation in CQI committee
- Participation in M&M committee
- Participation in weekly conference
- Resident portfolio and reflective statement
EDUCATIONAL OBJECTIVES – PGY 2
After successful completion of the PGY-1 year, the second year resident should be comfortable evaluating any patient who presents to the Emergency Department. During this year, the residents will be expected to develop their clinical acumen, sharpen their physical exam techniques and hone their procedural skills. Their organizational abilities should improve to the point that at least three to four patients can be managed simultaneously. Emphasis will also be placed on the importance of patient follow-up. The PGY-2’s demeanor should be calm and professional, reflecting their increasing competence and confidence in their abilities and in those of the staff around them. They will be expected to develop their teaching abilities at this stage as well. They will supervise PGY-1’s during procedures for which they have been credentialed; they will teach medical students, Physician Assistant students, and EMT students in the clinical setting.
PGY-2 residents will take active part in the presentation of cases in the weekly clinical case conferences, journal club, and M&M conferences. Research projects will begin during this academic year.
PGY-2 residents will be directly supervised by PGY-4 residents and faculty members, and will require their superior’s authorization for the admission, transfer or discharge of patients. A faculty member must sign all patient charts.
At the completion of this training year, the residents will demonstrate competence in and be able to :
- refine their history and physical exam skills
- document the medical record accurately and concisely
- recognize patients with potentially life-threatening conditions
- institute immediately life-saving therapy when necessary
- improve their ability to prioritize their activities
- formulate more extensive differential diagnoses on their patients
- plan appropriate work-ups based on their differential diagnoses
- plan admission, transfer, and discharges for their patients
- more appropriately utilize laboratory data and ancillary studies in the care of their patients
- carefully understand and utilize universal precautions
- more appropriately utilize specialty consultation
- function as a team member during resuscitations, and may act in leadership positions in supervised situations
Description of clinical experiences:
Second year residents should have experience and demonstrate competence in the following procedures:
- all procedures previously delineated for PGY-1’s
- tube thoracostomy
- arterial line placement
- endotracheal intubation
- venous cutdown
- closed diagnostic peritoneal lavage
- plastic suture techniques
- closed reduction of non-fractured displaced joints
- abdominal and pelvic ultrasound
- slit lamp examination
- removal of otic foreign bodies
- fracture reduction
- casting and splinting of non-displaced fractures
- intra-osseous infusion
- management of second and third degree burns
- rape-victim evaluation
Core Competencies
Patient care
- Procedural practice and teaching of these procedures
- Honing and demonstrating of physical exam skills
- Formulate treatment and disposition plans
- Triage of patients and prioritization of resuscitative efforts
- Participation in resuscitations
- Practice experience
- Skills labs
- Simulator time
- SDOT
Medical Knowledge
- Conference attendance and participation
- Topic review groups
- Webtests
- Inservice exam
- Bedside teaching rounds
- Responsibility for preparing case conferences
- Participation is skills labs
- Simulator time
- SDOT
Professionalism & Interpersonal
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Responsibility for presenting case conferences
Communication
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
System based practice
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Participation in CQI committee
- Participation in M&M committee
Practice based learning
- Simulator time
- Participation in CQI committee
- Participation in M&M committee
- Participation in weekly conference
- Resident portfolio and reflective statement
EDUCATIONAL OBJECTIVES – PGY 3
In the third postgraduate year the residents will grow in confidence while working independently. They will have an increased role in Junior Resident supervision, will refine their teaching skills, and carry out administrative tasks assigned by faculty members. In addition, PGY-3 residents will demonstrate increased competence in management of multiple critically ill or injured patients simultaneously. Research projects will continue this academic year. The third year resident will have the ability to make admission, transfer and discharge decisions, after discussing the case with a faculty attending physician. All charts must be co-signed by a faculty member. By the completion of this year of training they should be comfortable managing the full range of pathology that can present to an Emergency Department.
At the completion of this training year, the resident will demonstrate competence in and be able to:
- perform rapid, accurate histories and physical diagnoses on all patients presenting to the Emergency Department
- create comprehensive differential diagnoses for their patients
- create and carry out treatment and disposition plans for all patients presenting to the Emergency Department
- supervise the activity of more junior residents in their area
- conduct teaching/management rounds in all patient care areas, including the direct supervision of care provided by PGY-1 and 2 residents
- be an effective member of the Continuous Quality Improvement system
- be comfortable directing all patient resuscitation situations, and managing the critically ill and injured
- improve their lecturing and teaching skills
Description of clinical experiences:
- Third year residents should have experience and demonstrate competence in the following procedures:
- all procedures previously delineated for PGY-1 and 2
- pulmonary artery catheter placement
- extensor tendon repairs
- cricothyroidotomy
- umbilical catheterization
- supra-pubic bladder aspiration (pediatric)
- transthoracic echocardiography
- abdominal and pelvic sonography
- utilization of rapid-sequence and neuro-intubation techniques
- utilization of conscious sedation techniques
Core Competencies
Patient care
- Procedural practice and teaching of these procedures
- Demonstration of physical exam skills
- Supervision of junior practitioners
- Independent formulation of treatment and disposition plans
- Triage of patients and prioritization of patients
- Direction of resuscitative efforts
- Practice experience
- Skills labs participation
- Skills labs teaching
- Simulator time
- SDOT
Medical Knowledge
- Conference attendance and participation
- Supervision of select educational conferences
- Topic review groups participation
- Topic review groups mentoring
- Webtests
- Inservice exam
- Bedside teaching rounds
- Responsibility for preparing case conferences
- Participation in skills labs
- Simulator time
- SDOT
Professionalism & Interpersonal
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Responsibility for supervising case conferences
Communication
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Responsibility for supervising case conferences
System based practice
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Participation in CQI committee
- Supervision of M&M conference
Practice based learning
- Simulator time
- Participation in CQI committee
- Participation in M&M committee
- Participation in weekly conference
- Resident portfolio and reflective statement
EDUCATIONAL OBJECTIVES – PGY 4
In this last year of training the resident will receive progressive responsibility for the overall clinical and operational management of the Emergency Department. In essence, the PGY-4 should be ready to assume an attending-like position. With the guidance of Emergency Medicine faculty members, the Senior Resident will manage patient flow; train and assist in the evaluation of Junior Residents, Medical Students, Physician Assistant students and Pre-hospital personnel; assist with all admission, transfer and discharge decisions in their patient care area; and lead resuscitation situations. PGY-4 Residents will prepare and present curricula lectures; present cases at weekly discussions; run Morbidity and Mortality Rounds; and will assist Junior Residents in identifying cases for presentation and case reports. PGY-4 Residents will be able to independently admit, transfer or discharge patients after informing the faculty attending physician. All charts must still be co-signed by a faculty member.
At the completion of this training year, the resident will demonstrate competence in and will be able to:
- perform rapid, accurate histories and physical diagnoses on all patients presenting to the Emergency Department
- create comprehensive differential diagnoses for their patients
- confidently and competently create and carry out treatment and disposition plans for all patients presenting to the Emergency Department
- manage the activities of all more junior residents in their area, and be aware of all the patients in that area
- be comfortable conducting teaching/management rounds in all patient care areas, including the direct supervision of care provided by PGY-1 and 2 residents
- be an effective member of the Continuous Quality Improvement system
- be able to perform the administrative responsibilities of an Attending Physician
- be comfortable directing all patient resuscitation situations
- be comfortable managing critically ill and injured patients
- be an effective lecturer and teacher
Description of clinical experiences:
Fourth year residents should have had exposure and demonstrate competence in the following procedures:
- All procedures previously delineated for PGY-1, 2 and 3
- Emergency Department thoracotomy
- Transvenous pacemaker placement
- Fiberoptic laryngoscopy/intubation
Core Competencies
Patient care
- Procedural practice and teaching of these procedures
- Demonstration of physical exam skills
- Supervision of care by junior practitioners
- Independent formulation of treatment and disposition plans
- Triage of patients and prioritization of patients
- Direction of resuscitative efforts
- Practice experience
- Skills labs participation
- Skills labs teaching
- Simulator time
- SDOT
Medical Knowledge
- Conference attendance and participation
- Supervision of educational conferences
- Topic review groups mentoring
- Webtests
- Inservice exam
- Bedside teaching rounds
- Participation in skills labs
- Simulator time
- SDOT
Professionalism & Interpersonal
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Responsibility for supervising case conferences
Communication
- Modeling of behavior by faculty
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Responsibility for supervising clinical encounters
System based practice
- Observation during clinical shifts
- Web-eval system
- SDOT
- Simulator time
- Participation in CQI committee
- Supervision of M&M conference
Practice based learning
- Simulator time
- Participation in CQI committee
- Participation in M&M committee
- Participation in weekly conference
- Resident portfolio and reflective statement
OFF SERVICE ROTATIONS
PGY-1 OFF SERVICE ROTATIONS
Emergency GYN at KCHC (part of ED month)
ED-based Trauma Experience at KCHC
Obstetrics at KCHC
MICU at KCHC
Medicine at KCHC
All residents completing an Off-service rotation are required to meet with that rotation’s EM faculty liaison/coordinator for an exit interview in oral exam type format.
This shall serve as an evaluation of the rotation and the fulfillment of the educational expectations.
JUNIOR ULTRASOUND ROTATION
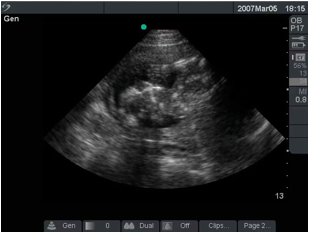
LENGTH: 2 WEEKS
YEAR OF TRAINING: PGY 1
LOCATION: KINGS COUNTY HOSPITAL EMERGENCY DEPARTMENT
FACULTY LIAISONS:
Dr. Kelly Maurelus Email: maurek01@gmail.com
Dr. Joshua Schechter Director, Resident Ultrasound Education
Cell: 646-281-1136
Email: joshschecht@gmail.com
OBJECTIVES:
To obtain clinical experience in managing emergent and urgent medical problems using ultrasound as a diagnostic tool.
To learn the differential diagnosis, workup, and management of patients presenting with common gynecologic complaints.
To become proficient at performing and interpreting the transabdominal and transvaginal pelvic ultrasound exam.
To become proficient in performing the AAA and FAST ultrasound exams.
SCHEDULE:
Clinical shifts: generally 10am-10pm on Mondays/Tuesdays/Thursdays/Fridays.
Ultrasound didactic shifts: generally 9am-10am on Thursday (film review) and on Wednesdays, after Conference.
You are expected to go to weekly conference on Wednesdays.
***YOU MUST E-MAIL DR. MAURELUS AND DR. SCHECHTER AT LEAST ONE WEEK PRIOR TO THE START OF YOUR ROTATION SO WE CAN ADJUST OUR SCHEDULES TO MEET WITH YOU,
ROTATION DESCRIPTION: Before starting each rotation please obtain the study materials from the Rotation Coordinator. Additionally there are still images and videos available at: http://www.sunysono.com
(username: suny password: s0n0)
At the beginning of the rotation the resident will meet with the faculty for a pre-test exam and specific instruction on the transvaginal and transabdominal pelvic ultrasound exam, the use and maintenance of the ultrasound machines, as well as receive didactic material such as books or image files.
During assigned clinical shifts in the KCH ER and under direct faculty supervision, the resident will evaluate patients who are triaged with gynecologic chief complaints. The resident will primarily pick up GYN-related charts. When there are no such patients to be seen, the resident will help out with the room and see other patients, with an eye to remaining available to pick up new GYN-related patients as they come in.
The resident will evaluate GYN patients during these clinical shifts as per usual clinical care (i.e., H&P, differential diagnosis, ordering diagnostic tests and therapeutics, obtaining and following consults, and disposition), with the addition of performing a pelvic ultrasound exam whenever appropriate. These patients should be presented to and followed by a faculty attending that is working clinically during the shift.
All studies MUST be done under the DIRECT SUPERVISION of a provider credentialed in emergency ultrasound (faculty or fellow). When done for a clinical indication, the results MUST be documented in Quadramed by ED QuickNote or as otherwise directed. Additionally, ultrasound images should be saved with results documented on the Ultrasound Data Sheet (found on clinicalmonster.com). The ultrasound faculty will critique these during weekly film review sessions. The data sheets must be turned in at the end of the rotation. We require at least 25 documented and approved in each application of emergency ultrasound (AAA, FAST, and pelvic ultrasound – transabdominal and transvaginal combined), so every exam should be documented.
The rotating intern will be responsible for maintaining all appropriate supplies and keeping the Ultrasound machine clean and in its designated area. The machine should be turned on and checked at the beginning of each shift. Any problems with the machine should be immediately reported to the Emergency Ultrasound Attending on schedule that day. If the attending cannot be reached, the Director of the Division (Dr. Secko) must be contacted.
In case of an unexpected absence the resident must contact both the Chief Resident, the Director of Resident Ultrasound Education, and the Director of the Emergency Ultrasound Division.
ACEP Quizes:
Please complete the following quizzes during the rotation. The results should be emailed to Dr. Maurelus or Dr. Schechter. They can be found at the WEBSITE: www.emsono.com/acep
- Physics
- OB/GYN
- FAST
- Aorta
EVALUATION:
Upon completion of the rotation, the resident will be evaluated based on his/her attendance, motivation, didactic knowledge and procedural skills. There will be an exam consisting of written questions and videos covering the assigned knowledge base (basic ultrasound physics, general OB/GYN pathology, and AAA/FAST/pelvic ultrasound exams). The resident will also receive feedback during the rotation. The evaluation will be completed in new innovation will be reviewed by the residency directors. The resident will have access to the evaluation through new innovations. The resident will be also asked to evaluate the rotation and provide suggestions for improvement. All interns are required to complete written examination at end of rotation.
TAPE REVIEW:
Each resident needs to be present at tape review on Thursday’s at 9am in the US conference room.
Each resident is expected to have manual data sheets completed prior to each tape review of all GYN pts seen. Furthermore, each intern is required to present one ultrasound article at tape review.
ED-BASED TRAUMA
Meeting Place: KCH ED
Contact Number: EM Chiefs
Daily Rounds: ED morning report
Schedule: The EM Trauma intern will be expected to function the same as our regular EM interns but will have a different shift distribution. You will also be scheduled for an intensive 1-day session of Trauma skills-stations and lectures during orientation.
Description of rotation:
During the Trauma rotation, the PGY-1 Emergency Medicine Residents will rotate through the KCH ED for a 2-week time period. During that time, they will be responsible for 5 CCT shifts and 4 Pod A shifts. They should try to focus on traumatized/injured patients but can and should see any patient that presents to their area that needs to be cared for.
In addition to this 2-week block, each PGY 1 will attend a “Focused Trauma Workshop” spanning 1 day during your orientation month. During this time period, the resident will have multiple activities to complete. The days will begin with a number of trauma-oriented lectures. They will then participate in multiple hands-on small group learning sessions involving critical trauma skill sets and will be exposed to multiple simulation cases involving traumatized patients. Lastly, there will be a reading list made available on the KCH EM web site where a number of trauma-oriented PDF papers can be downloaded. The resident is responsible for reading these papers prior to the completion of their PGY 1 residency year.
The Emergency Medicine Resident will have direct patient care responsibility: In the Emergency Room, they will be doing what all of the other PGY 1’s are doing that month with the exception being that they are supposed to be concentrating on traumatized patients. Just like the other PGY 1’s in the ED that month, the resident rotating on trauma will have to attend regular Wednesday didactic EM Conference and morning reports according to the usual rules for absence. During the shifts in the Main ED, the resident will focus on injured patients. If no injured patients are waiting to be seen, then the resident will see ED patients with any chief complaint.
All trauma resuscitations are to be documented in New Innovations for credit.
At the completion of this rotation the resident will demonstrate competence in the following:
MEDICAL KNOWLEDGE, PATIENT CARE
- Recognition of the various stages of traumatic shock, including its earliest manifestations (PC,MK)
- The principles and endpoints of resuscitation, including the roles of:
-Crystalloid volume replacement
-Colloidal volume replacement
-Blood volume replacement
-Inotropic support (PC,MK)
- The initial assessment of the multiply injured patient (ABC’s) (PC,MK)
- Identification and treatment of immediately life-threatening injuries after the initial assessment (PC,MK)
- The role of radiographic studies in the initial and subsequent management of the injured patient (PC,MK)
- Common injury patterns associated with penetrating head trauma (PC,MK)
- Common injury patterns associated with blunt head trauma (PC,MK)
- How the presence of a closed head injury impacts management of a multiply injured patient (PC,MK)
- Management of elevated intracranial pressure (PC,MK)
- The anatomic zone system of the neck, and appropriate work-up and management of a penetrating injury to each of the zones (PC,MK)
- Indications for operation in penetrating chest trauma (PC,MK)
- Identification and management of patients at risk for pericardial tamponade (PC,MK)
- Recognition of a widened mediastinum on X-ray, its significance and work-up (PC,MK)
- Physiologic scoring (PC,MK)
- Evaluation of blunt abdominal trauma including:
-Physical exam
-Diagnostic peritoneal lavage
-Abdominal CT scanning
-Abdominal sonography
-Laparoscopy
-Non-operative management (PC,MK)
- Classification of pelvic fractures and radiographic studies used for their diagnosis (PC,MK)
- Diagnosis and management of the bleeding associated with pelvic trauma, including:
-external fixation
-angiography (PC,MK)
- Diagnosis and management of urologic complications associated with pelvic trauma (PC,MK)
- Evaluation and management of gross hematuria following trauma (PC,MK)
- Signs of peripheral vascular injury and the indications for angiography and operative management (PC,MK)
- Special concerns in the care of patients with spinal injuries (PC,MK,SBP)
- Special concerns in diagnosis and management of elderly injured patients (PC,MK,SBP,P)
- Importance of long bone fractures in the short and long term outcome of the multiply injured patient (PC,MK)
- Appropriate utilization of specialty consultants in the management of multiply injured patients (PC,MK,C,P,SBP)
- The concept of triage within the confines of available resources, including recognition of non-salvageable patients (PC,SBP,MK)
- Pulmonary artery catheterization for hemodynamic monitoring
- Identification of potential organ donors and their management to maximize yield of organ procurement(PC,SBP,P,C)
- Patient discharge and transfer decisions, including formulation of long-term care plans for patients with spinal cord injuries and major disability(PC,P,C,SBP)
- Compassionately interact with patients and their families during the stress of illness and death, including the ability to obtain DNR orders(PC,P,C)
- The patterns and demographics of the urban trauma patient(PC,SBP,PBL)
Educational Expectations:
The following topics should be covered in the resident’s reading during this rotation:
ATLS Hemodynamic monitoring
Volume resuscitation (crystalloid and colloid)
Neuro-intubation Resuscitation with blood products
Rapid sequence intubation Inotropic support
Intubation with cervical spine trauma SVO2 as a guide to resuscitation
Intubation with facial trauma Lactate and base deficit to monitor perfusion deficit
Mechanical ventilation Shock(hemorrhagic,neurogenic,cardiogenic)
Spinal trauma Physiologic scoring
Spinal shock Tissue ballistics
Penetrating and blunt thoracic trauma Trauma in pregnancy
Penetrating and blunt abdominal trauma Trauma in the elderly
Penetrating and blunt neck trauma Pediatric trauma
Head trauma
Glasgow Coma Scale
Pelvic trauma
Facial trauma
Long bone fractures (open and closed)
Vascular injury
OBSTETRICS
Meeting Place: S building 5th floor
Daily Rounds: 9am
Schedule: Contact Ms. Stephanie Goeloe (OB residency coordinator) (718) 270-3320.
If unable to reach Ms. Goeloe, the Chief resident of OB at KCH should be able to help. You can reach the OB Chief Resident through the KCHC operator at (718) 245- 3141
Educational Objectives:
PGY-1 Emergency Medicine residents will spend a two-week block on the Obstetrics in-patient service at Kings County Hospital. Residents will also rotate through the outpatient clinics. The Emergency Medicine Residents will be under the direct supervision of an Obstetrics/Gynecology Senior or Chief Resident and Attending Physician. They will act in the role of a PGY-1 OB/GYN Resident, providing direct patient care, and assisting with in-patient and Emergency Department consultation. They will also assist in the operating rooms. The Emergency Residents will attend the Department of Gynecology’s daily conferences and monthly Grand Rounds, as well as Emergency Department Educational events, if patient care requirements allow. The purpose of this rotation to perform at minimum the 10 deliveries required by the RRC for graduation. All deliveries are to be documented in New Innovations for credit.
At the completion of this rotation, the resident will demonstrate competence in and be able to:
Evaluate and treat the patient with pre-eclampsia/eclampsia (PC,MK)
Make admission, transfer and discharge decisions on OB patients (PC,MK,C,SBP,P)
Utilize laboratory data and ancillary studies appropriately in the care of OB patients (PC,MK)
Utilize in-patient consultation appropriately (PC,MK,C,P,SBP)
Compassionately interact with patients and their families during the stress of illness and death (PC,C,P)
Description of clinical experiences:
Residents will have experience in and demonstrate competence in the following procedures:
- Vaginal deliveries
- Assisting in C-sections
- Monitoring of patients in labor
- Management of the ecclamptic patient
- Management of episiotomies
- Culdocentesis
- Assisting in the operating room
- Pelvic sonography
- Pelvic examination
- Assisting with the treatment of incomplete and complete abortions
- Appropriate bacterial and viral culture techniques
- Repair of vaginal lacerations
- Removal of vaginal foreign bodies
Description of didactic experiences:
The residents will participate in the daily, weekly, and monthly OB/GYN conferences as well as the Emergency Medicine conferences if it is does not interfere with patient care requirements.
The following topics should be covered in the Resident’s reading during this rotation:
Pelvic and abdominal pain Abnormal vaginal bleeding
Ovarian cysts and rupture thereof Tubo-ovarian abscess
Spontaneous abortion Threatened abortion
Endometriosis Pelvic inflammatory disease
Ectopic pregnancy Uterine incarceration
Ovarian torsion Mittelschmerz
Vaginitis/vaginosis/vulvitis Urinary tract infection
Sexually transmitted disease Atrophic vaginitis
Infertility Vaginal foreign bodies
Sexual assault Contraception
Drug and radiation exposure in pregnancy Diagnosis of pregnancy
Nausea and hyperemesis gravidarum Premature rupture of membranes
Vaginal bleeding in early pregnancy Molar pregnancy
Contraception Hysterectomy
Pelvic relaxation Amenorrhea
MICU
Meeting Place: KCH MICU D building
Contact Number: (718) 245-3774 (KCH) , MICU # 718-245-7580
Daily Rounds:. Usually at 7am in D3South Conference room. Contact KCH Medical Chief Resident for the block 917-760-1320, 917-760-1321. Ezra Miller Ezra.Miller@downstate.edu, Andrew Persits Andrew.Persits@downstate.edu,
Schedule: Contact the KCH Medical Chief Resident: Andrew or Ezra at least 4 weeks before the start of the rotation.
EM Faculty Liaison: Dr. Claritza Rios Cell 347-346-0030
Special Considerations:
The Medical Intensive Care Unit at Kings County Hospital is a four week rotation for PGY-1 Emergency Medicine Residents. The Emergency Medicine Resident will function as a PGY-1 Internal Medicine Resident, providing direct patient care. A Senior Medical Resident, Critical Care Fellow and the Intensive Care Unit Attending Physician will supervise the Emergency Medicine Resident. The Emergency Medicine Resident will attend daily Attending Rounds, daily lectures with the Department of Internal Medicine, weekly Critical Care Conferences, monthly Internal Medicine Grand Rounds, and participate actively in the monthly Emergency Medicine / MICU interdisciplinary conference. The resident must attend the weekly Emergency Medicine Departmental conference.
At the completion of this rotation, the resident will demonstrate competence in and be able to:
Perform a comprehensive history and physical examination on critically ill patients(MK,PC)
Develop differential diagnoses for life-threatening problems, and create cohesive care plans based on these diagnoses(MK,PC,PBL)
Manage critically ill patients in an intensive care unit setting(MK,PC,PBL)
Make admission, transfer and discharge decisions for patients with life-threatening and potentially life-threatening illness(MK,PC,C)
Appropriately utilize and interpret invasive monitoring(MK,PC)
Appropriately utilize and interpret culturing techniques, results and use of antibiotics(MK,PC)
Utilize laboratory data and ancillary studies appropriately in the care of critically ill patients(MK,PC,SBP)
Utilize in-patient consultation appropriately(MK,PC,C,P,SBP)
Compassionately interact with patients and their families during the stress of illness and death(PC,P,C)
Description of clinical experiences:
Residents should have experience with and demonstrate competence in the following procedures on this rotation: (MK,PC)
Airway management and endotracheal intubation
Placement and care of central venous catheters
Placement and care of arterial catheters
Placement and care of pulmonary artery catheters
Interpretation of Swan-Ganz-catheter readings
Utilization of oxygen delivery devices and mechanical ventilators
Lumbar puncture
Arterial blood gas sampling and analysis
Abdominal paracentesis
Thoracentesis
Chest tube placement
Placement of esophageal/gastric balloons
Description of didactic experiences: (MK,PC)
The Emergency Medical resident will actively participate in the interdepartmental conferences.
The following topics should be covered in the resident’s reading during this rotation:
Airway management and endotracheal intubation
Mechanical ventilation ACLS
Interpretation of invasive monitoring Drug induced paralysis
ARDS Asthma/COPD
Pneumonia Meningitis
Opportunistic infection Super-infection
Broad spectrum antibiotics Acute renal failure
Hemodialysis/peritoneal dialysis Gastrointestinal hemorrhage
Intracerebral bleeding/CVA Hepatic encephalopathy
Shock Sepsis
Uremic encephalopathy Anticoagulant therapy
Pulmonary embolism Coma/brain death examination
Cardiogenic pulmonary edema Dysrhythmias
Fever Acid base derangements
Electrolyte abnormality Nutrition: parenteral and enteral
Disseminated intravascular coagulation Hemolysis
INTERNAL MEDICINE FLOORS AT KCH
Meeting Place and Time: D Building 7Th floor North- Conference Room at 7am
Pagers for KCH Medical Chief Residents: Ezra Miller Ezra.Miller@downstate.edu,
Andrew Persits Andrew.Persits@downstate.edu 917-761- 1320
917-761- 1321
Schedule and Inquiries: Contact medicine chief resident at least 3-4 weeks before the start of the rotation:
EM Faculty Liaison: Dr. Claritza Rios Cell: (347) 346-0030
Educational Objectives:
PGY-1 Emergency Medicine Residents will rotate for a four-week block on the in-patient Medical Services at the KCHC. The Emergency Medicine Residents will be integrated into the schedule of the Department of Medicine by the respective Chief Medical Residents. The Emergency Medicine Residents will function in the role of a PGY-1 Internal Medicine Resident, and will have direct patient care responsibility. They will be under the direct supervision of a PGY-3 Medical Resident and Internal Medicine Attending Physician. Residents will also attend daily attending rounds, daily educational conference, weekly Medicine Department Grand Rounds and the monthly Morbidity and Mortality Review.
At the completion of this rotation the resident will be familiar with and demonstrate competence in:
- Performance of a comprehensive history and physical examination on acutely and chronically ill patients(PC,MK)
- Development of an integrated problem list for patients, including detailed differential diagnoses.(MK,PC)
- Management of complex medical problems on an acute and chronic basis.(MK,PC,SBP)
- Transfer and discharge planning.(SBP,PC,P)
- Utilization of laboratory data and ancillary studies in the care of internal medicine patients(MK,PC)
- Blood and body fluid precautions(MK,SBP)
- Necessary precautions for Tuberculosis and other airborne pathogens(PC,MK,SBP)
- Appropriate utilization of specialty consultation(C,P,PC,MK)
Medical Knowledge and Patient Care:
- Management of the immune-compromised patient
- Management of the patient with accelerated hypertension, and hypertensive urgencies
- Management of congestive heart failure
- Management of asthma/COPD
- Management of gastrointestinal bleeding
- The evaluation and management of fluid and electrolyte disorders
- The evaluation and management of hypothermia and hyperthermia
- The evaluation and treatment of suspected spinal cord compression
- Management of diabetes: its acute (DKA, Hyperosmolar Coma), and chronic (leg ulcers, renal failure, neuropathy, retinopathy) manifestations
- The evaluation and treatment of acute and chronic renal failure
- The metastatic work-up
- Nutrition: parenteral and enteral
- Initial management of myocardial ischemia
- Recognition and treatment of the initial stages of septic shock
- The differential diagnosis of wide-anion gap and non-anion gap metabolic acidosis
- Management of pneumonia
- Diagnosis and management of patients with CNS and systemic infections
- Evaluation and treatment of patients with vasculitis and connective tissue disorders; lupus, scleroderma, mixed connective tissue disorder
- Development of the Doctor-Patient relationship as the resident interacts with patients and their family’s during the stress of illness and death
Description of clinical experiences:
Residents should have experience and demonstrate competence in the following procedures on this rotation:
- Advanced Cardiac Life Support
- Emergent airway management
- Diagnostic lumbar puncture.
- Abdominal paracentesis
- Peripheral blood smear analysis
- Thoracentesis
- Arterial blood gas sampling and its analysis
- Lymph node aspiration for cytology diagnosis
- Peripheral IV catheter placement
- Central IV placement and care
- Urinalysis
- Blood and tissue culture techniques
- Viral culture techniques
- Nasogastric intubation
- Debridement of decubitus ulcers
Description of didactic experiences:
The resident will attend all lectures offered by the Internal Medicine department.
The following topics should be covered in the resident’s reading during this rotation:
Hypertension Pulmonary embolism
Diabetes insipidus Deep vein thrombosis
Diabetes mellitus Malignancy
Diabetic ketoacidosis Paraneoplastic syndromes
Diabetic hyperosmolar state Lymphoma/leukemia
Electrolyte disturbances Metabolic acidosis
Acute and chronic renal failure Asthma/COPD
Anemia Pneumonia
Hemolysis Sepsis
AIDS TB
Brain abscess Infectious diarrhea
Connective tissue disorders Vasculitis
TTP ITP
Acid-peptic disorders Spinal cord compression
Pancreatitis Hepatitis
Upper GI bleeding Lower GI bleeding
Congestive heart failure Myocardial ischemia
Atrial fibrillation Atrial tachycardias
Sarcoidosis
PGY-2 OFF SERVICE ROTATIONS
Airway Management
ENT
Research
CCU at LICH
NICU at UHB
SICU at KCHC
Stroke at LICH
Orthopedics/FT at KCH
AIRWAY MANAGEMENT
Location: KCHC OR Room S3-76 (S-Building 3rd floor)
Faculty Liaison: Dr. Stephan Rinnert
Contact: Dr. Adwoa Essuman x 4502
Dr. Lara Delong x 4502
Dr. Dawodu x 4502
Structure:
The rotation takes place during a two-week block during the second year. During this time the residents will report to the clinical director at 7 a.m. every weekday. The resident will have the opportunity to develop his/her airway management skills under close supervision in the controlled setting of the OR.
The resident should also schedule a time with Dr. Silverberg, Stetz or DaCoasta to do a practical airway lab. It is not necessary to complete the lab during this 2-week period, but should be completed. This workshop occurs in 2 stages and practices the mechanics of intubation and LMA placement as well as the use of rescue devices.
Goals and Objectives:
- The resident will develop and demonstrate competence in the following clinical skills: (MK,PC)
- Airway opening techniques.
- Use of oral and nasal airways.
- Bag valve mask ventilation.
- Safe administration of sedatives and muscle relaxants.
- Laryngoscopy anatomy and technique.
- Orotracheal intubation.
- Techniques for confirming endotracheal tube placement.
- Basic ventilation parameters.
- The use of the laryngeal mask airway for primary ventilation and airway salvage.
- The resident will demonstrate competence in and detailed knowledge of the following topics:
- Airway anatomy and physiology in adults and children.
- The pharmacology of commonly used sedative and paralytic agents.
- Airway management in trauma.
- Airway management in the patient with suspected intra-ocular of intra-cranial injury.
- Airway management in children.
- Indications for primary and salvage intubation with the laryngeal mask airway (including the intubating laryngeal mask airway).
- Familiarity with the combitube SA.
Reading Suggestions:
- The text for this course is The Airway Cam Guide to Intubation and Practical Emergency Airway Management, by Rich Levitan MD. This is a short paperback text written by a national leader in the field of airway management. It covers all of the areas germane to the rotation objectives. This book in the department library.
- The residents will be expected to view the Airway Cam videos. These were also developed by Rich Levitan, M.D. and take the resident through airway anatomy, use of different laryngoscopic equipment, different intubation techniques, and the management of the difficult airway. The total video time is approximately one and a half hours.
Evaluation:
At the end of each rotation, the supervising faculty will complete the evaluation form provided by the Department of EM and will discuss it with the resident. An evaluation of the rotation from the resident will also be solicited. Both of these will be placed in the resident’s folder and reviewed by the residency directors.
CCU
Meeting Place: CCU , NS26 2nd floor UHB
Schedule: Internal Medicine Chief Residents, Kalia Skeete 917-761-1323
EM Faculty Liaison: Claritza Rios 3473460030
Educational Objectives:
The Coronary Care Unit at UHB will be the PGY-2 Emergency Medicine Resident’s introduction to the cardiac patient. They will be providing direct patient care in the CCU. Emergency medicine residents will be supervised by cardiac fellow, or a cardiology attending. The Emergency Medicine Resident will attend daily Attending Rounds and Unit lectures as well as all daily lectures with the Department of Internal Medicine.
Day-to-Day Assignments: q4 24 hour overnight call, work hours on call days7am-10am, work hours on non-call days7 AM to 5 PM, off on post-call days plus on additional day per week
Typical Day: 7 AM to 8:00 AM – Sign out rounds, work rounds, and notes, 8 AM to 10 AM- Attending management and teaching rounds, 12 Noon- Cardiology or Medicine conference (Lunch), 1 PM to 4:00 PM afternoon work rounds, check results and consultations etc. 4-5 PM- sign out rounds
Conferences: Daily Internal Medicine Noon conference- see monthly schedule
At the end of your CCU rotation you will be required to turn in one interesting EKG that will eventually be posted on the blog site. If you do not have the ability to scan the EKG into digital format, you can ask Dr. Silverberg or anyone else to help you. The EKG should portray some interesting pathology that will spark an academic conversation. These images should be turned in to Dr. Khadpe (jkhadpe@gmail.com) or someone he designates. Images need to be accompanied by an “answer” explaining why the image is important.
At the completion of this rotation, the Resident should demonstrate competence in and be able to:
- Perform a comprehensive history and physical examination on cardiac patients (PC, PROF)
- Develop differential diagnoses for chest pain and cardiac problems, and create cohesive care plans based on these diagnoses (PC, MK, SBP)
- Manage cardiac patients in an intensive care unit setting (SBP, PC, MK)
- Make admission, transfer and discharge decisions for patients with cardiac disease and potentially life-threatening illness (SBP, PC)
- Diagnose and treat supraventricular and ventricular dysrhythmias (PC, MK)
- Evaluate and treat hypertensive crisis (PC,MK)
- Evaluate and manage myocardial ischemia (PC.MK)
- Evaluate and manage acute myocardial infarction and its complications, including wall rupture, valve failure, congestive failure, dysrhythmias and pericarditis (MK, PC, SBP)
- Evaluate and manage dissecting thoracic aortic aneurysm (MK,SBP,PC)
- Evaluate and manage hypertrophic cardiomyopathy (MK,PC)
- Evaluate and manage cardiogenic pulmonary edema (MK,PC)
- Evaluate and manage class III and IV congestive cardiomyopathy (MK,PC)
- Evaluate and manage infective endocarditis (MK,PC)
- Evaluate and manage failed or infective prosthetic heart valves (MK,PC)
- Evaluate and manage pericardial tamponade (MK,PC, SBP)
- Evaluate and manage pericarditis (MK,PC)
- Run a cardiac arrest situation (MK,PC, PROF, COM, SBP)
- Appropriately utilize thrombolytic therapy and manage its complications (PBL, SBP)
- Interpret EKG’s quickly and accurately (MK,PC)
- Appropriately utilize and interpret invasive monitoring (MK, SBP, PC)
- Utilize laboratory data and ancillary studies appropriately in the care of critically ill patients (MK, PC, SBP, PBL,)
- Utilize in-patient consultation appropriately (COM, SBP, PROF)
- Compassionately interact with patients and their families during the stress of illness and death (PROF, COM)
Description of clinical experiences: (MK,PC)
Residents should have experience and demonstrate competence in the following procedures on this rotation:
- Advanced Cardiac Life Support
- Airway management and endotracheal intubation
- Placement and care of central venous catheters
- Placement and care of arterial catheters
- Placement and care of pulmonary artery catheters
- Utilization of oxygen delivery devices and mechanical ventilators
- Arterial blood gas sampling and interpretation
- Exercise stress testing
- 24 hour ambulatory monitoring
- Bedside echocardiography
- Alternative EKG lead placement for the diagnosis of dysrhythmias and infarction
- Internal and external temporary pacemaker placement
Description of didactic experiences: (MK,PC, PBL, SBP)
The following topics should be covered in the Resident’s reading during this rotation:
Chest pain (differential diagnosis of) Coronary artery disease
Hypertensive crisis Dissecting aortic aneurysm
Coronary artery spasm Cardiogenic pulmonary edema
Acute myocardial infarction-diagnosis Treatment of AMI
Myocarditis Pericarditis
Pericardial tamponade Congestive heart failure
Restrictive cardiomyopathy Hypertrophic cardiomyopathy
Congenital heart disease Nitrates/Beta-blockers /Digoxin
Calcium channel blockers Heparin/coumadin
Thrombolytic therapy Pacemakers
Dysrhythmias-supraventricular Dysrhythmias & Anti-dysrhythmics
ACLS protocol Cardiac catheterization
Echocardiography Electrophysiologic studies
Stress testing Nuclear cardiology
Invasive pressure monitoring Intra-aortic assist devices
Heart blocks Wolff-Parkinson-White syndrome
All residents completing an Off-service rotation are required to meet with that rotation’s EM faculty liaison/coordinator for an exit interview in oral exam type format.
This shall serve as an evaluation of the rotation and the fulfillment of the educational expectations.
NICU
Meeting Place: 7 am NS35, NICU, 3rd Floor UHB
EM Faculty Liaison: Dr. Antonia Quinn
Contact : Dr. Gloria Valencia, Director NICU, Vice Chair UHB Clinical Services
Schedule: Email requests to Pediatrics Chief Residents (pedschiefs@hotmail.com)
and Dr. Valencia (Gloria.Valencia@downstate.edu) who makes the NICU schedule (2 months ahead of time)
Educational Objectives:
As a PGY-2, the resident will rotate for four weeks in the NICU in the role of a junior resident. The resident will work under the supervision of an Attending Neonatologist. The resident will also be present at “difficult” or complicated deliveries and gain experience in neonatal resuscitation and stabilization.
- To become competent in the initial resuscitation of the premature and term neonate during both complicated and routine deliveries. (MK,PC)
- To understand and manage the unique respiratory and nutritional needs of the premature infant. (MK,PC)
- To properly order and interpret laboratory and radiographic tests for the purpose of diagnosis and treatment of the neonate in the intensive care unit. (MK,PC,SBP)
Clinical Experience:
The resident will demonstrate competence in the evaluation and management of the following neonatal disorders:
- Esophageal reflux
- Aganglionic megacolon
- Congenital GI lesions
- Acquired GI conditions (NEC)
- Hernias
- Malrotation of bowel
- Dysrhythmias
- Congenital heart disease
- Hypoglycemia
- Neonatal Jaundice
- Anemias
- Meningitis
- Neonatal seizures
- Hydrocephalus
- Congenital cysts
- Bronchopulmonary dysplasia
- Bacterial pneumonia
- Perinatal and congenital infections
- Congenital kidney abnormalities
- Undescended testes
- Vaccination
- Pharyngeal – Tracheal lumen airway
The resident will understand and demonstrate competence in the mechanics of assisted ventilation and the proper methods for monitoring adequate oxygenation:
- Mechanical ventilation
- End-tidal CO2 monitoring
- Pulse oximetry
The resident will demonstrate competence in the following procedures:
- Umbilical vein catheterization
- Umbilical artery catheterization
- Familiarity with chest tube placement in neonates
- Use of paralytic and sedation agents
- Orotracheal intubation
Description of didactic experiences:
The resident will attend all educational conferences and meetings while on the NICU Service. The resident will be responsible for the list of suggested readings for the NICU Rotation in addition to any provided by the NICU Service. The resident will be fully incorporated into the NICU Care Team and participate in all rounds, conferences and didactics including Perinatology Conference and Neonatal Morning Report weekly. Attendance at the Wednesday Emergency Department Conferences will be at the discretion of and with the permission of the NICU attending on service if patient care needs allow.
ENT
Meeting place: ENT Clinic
Contact Number: (718) 245-3470
Schedule: 1:00pm until clinic ends (usually 4-5pm),
weekdays except Thursdays
EM Faculty Liaison: Mark Silverberg
Educational Objectives for ENT rotation:
PGY-2 Emergency Medicine Residents will rotate for two weeks on the Otolaryngology service at Kings County Hospital. (During this two weeks you should also be working on a research project with the research team in the mornings when you are not in ENT clinic.) The Emergency Medicine Residents will be integrated into the clinic schedule of the Department of Otolaryngology by the chief or Chairman of ENT.
The EM Resident will function in the capacity of a junior Otolaryngology Resident. The resident will see patients in the clinic, in the operating room, as a consultant to the Emergency Department, on the general floors and in the critical care units of the hospital. The Resident will be under the direct supervision of an Otolaryngology Attending Physician and senior Otolaryngology residents. Residents can attend daily attending rounds, daily educational conferences, and weekly Otolaryngology Grand Rounds. They will also attend all Emergency Medicine Department Conferences and educational events. Wednesday afternoons are to be spent in ENT clinic or doing ENT consults. Thursday afternoons are free time to catch up on reading.
At the completion of this rotation the resident will be familiar with and demonstrate competence in the following concepts:
Examination of the head, ears, nose, throat and neck (PC)(MK)
Normal and abnormal anatomy (MK)
Management of nasal bleeding (PC)
Management of trauma to the face (PC)(MK)
Management of trauma to the ears (PC)(MK)
Management of trauma to the nose (PC)(MK)
Management of trauma to the mouth (PC)(MK)
Management of trauma to the neck (PC)(MK)
Recognition, identification and management of tumors of the head and neck (PC)
The evaluation and treatment of hoarseness (PC)
Management of airway emergencies (PBL, PC, MK)
Evaluation of acute and chronic hearing loss (MK)
Evaluation and treatment of the patient with extra-cranial infection of the head including: sinusitis, otitis externa, otitis media, facial cellulitis, Ludwig’s angina, pharyngitis, retropharyngeal abscess, and acute epiglottitis (PBL, MK, PC)
Evaluation and treatment of infections of the neck (PC, MK)
Care of the tracheostomy patient (PC, MK, SBP)
The role of an Otolaryngology Consultant on both emergent and non-emergent patients (SBP, COM, PROF)
Appropriate admission of patients to the hospital on the Otolaryngology service (SBP, PC, COM)
Develop the Doctor-Patient relationship as the resident interacts with patients and their families (PROF, COM, PBL)
Description of clinical experiences: (PC, MK, PBL)
Residents should have experience and demonstrate competence in the following procedures on this rotation:
Control of epistaxis, including anterior cauterization
Anterior and posterior nasal packing
Topical anesthesia
Laryngoscopy: indirect (mirror)
Laryngoscopy: direct (fiberoptic nasopharyngolaryngoscopy)
Management of nasal lacerations
Management of nasal fractures and other nasal trauma
Management of injuries to the external ear
Management of injuries to the middle and inner ear
Management of common neck wounds
Incision and drainage of oral, pharyngeal and cervical abscesses
Description of didactic experiences:
The following topics should be covered in the resident’s reading during this
rotation:
Acute hearing loss Sinusitis
Otitis Media Facial Cellulitis
Otitis Externa Ludwig’s Angina
Ear Foreign bodies Salivary Gland Problems
Epistaxis Maxillofacial fractures
Nasal Fractures Odontogenic Infections
Rhinitis Epiglottis
Acute Upper Airway Obstruction Cricothyrotomy
Emergency Tracheostomy Endotracheal Intubation
Post adenotonsillectomy Bleeding Peritonsillar Abscess
Retropharyngeal Abscess Parapharyngeal Abscess
Pharyngitis Upper Airway Foreign Bodies
Ruptured Tympanum Vertigo
Tracheostomy Tracheostomy Tube Placement
Cholesteotoma Mastoiditis
Tumors of the head and neck
SICU
Meeting Place: SICU D3
Contact Number: (718) 245-4522/3982
Daily Rounds: 6:30 am daily
Schedule: The on-call schedule is made by the Department of Surgery. EM residents will have similar call responsibilities as surgical residents
Residents will NOT be required to attend the weekly ED educational conferences
EM Faculty Liaison: Dr. Bonny Baron
Educational Objectives:
PGY-2 Emergency Medicine Residents will spend four weeks in the SICU at Kings County Hospital. The Emergency Medicine PGY-2 resident will function as PGY-2 Surgical Residents. They will have critical care patient responsibilities under the direct supervision of a PGY-4 general surgery resident and general surgery/trauma/critical care attending physicians. While on rotation they will attend daily patient care work rounds and attend daily educational rounds. They will attend the weekly trauma conference.
At the completion of this rotation, the Resident will demonstrate competence in and will be able to:
- perform initial ICU assessment of critically ill and injured patients using history and physical examinations
- understand the indication for invasive monitoring and its goals and complications
- master the principles of shock resuscitation especially as defined by oxygen transport parameters
- understand the indications and complications of inotropes, vasopressors, preload reducing agents, and afterload reducing agents
- understand the proposed mechanisms of multiple organ failure including mediators of the inflammatory response and therapies designed to modulate this response
- understand the modifications necessary in resuscitation of patients with closed head injuries
- master the indications for, and use of mechanical ventilators including the ability to wean a patient from a ventilator
- understand the indications for and use of enteral and parenteral nutritional support
- identify the signs and symptoms of early sepsis and the work-up necessary for full investigation
- understand the rationale for antibiotic use in the Intensive Care unit: prophylactic and therapeutic
- assess renal function in critical illness, including the use of creatinine clearance, free water clearance and fractional excretion of sodium as diagnostic tools
- understand the evaluation of hepatic function in critical illness
- manage life threatening gastrointestinal bleeding
- mange drainage tubes
- understand the mechanism and treatment of common coagulopathies associated with organ failure in critical illness
- compassionately interact with patients and their families during the stress of illness and death, including the ability to obtain DNR orders
Description of clinical experiences:
Residents demonstrate competence in the following procedures on this rotation:
- Cardiopulmonary resuscitation
- Airway management and endotracheal intubation (nasal and oral)
- Management of ICP monitors and ventricular drains
- Placement and care of central venous catheters
- Placement and care of arterial catheters in all sites
- Placement and care of pulmonary artery catheters
- Utilization of oxygen delivery devices and mechanical ventilators
- Lumbar puncture
- Obtaining cultures from all sites and tissues
- Placement of enteral feeding tubes
- Arterial blood gas sampling and analysis
- Abdominal paracentesis
- Thoracentesis
- Tube thoracostomy
- Placement of esophageal/gastric balloons
- Assisting in performance of peritoneal dialysis and continuous A-V hemofiltration
- Assisting in endoscopic examination of the upper and lower GI tracts
Description of didactic experiences:
The residents will attend daily, weekly and monthly surgical/critical care/ trauma conferences.
The following topics should be covered in the resident’s reading during this rotation:
Airway management ACLS
Mechanical ventilation High frequency ventilation
Interpretation of invasive monitoring ARDS
Post-operative management Wound management
Pneumonia A-V hemofiltration
Blood product usage Super-infection
Broad-spectrum antibiotics Acute renal failure
Hemodialysis/peritoneal dialysis Gastrointestinal hemorrhage
Intracerebral bleeding/CVA Hepatic encephalopathy
Shock Sepsis
Uremic encephalopathy Anticoagulant therapy
Pulmonary embolism Coma/brain death examination
Cardiogenic pulmonary edema Dysrhythmias
Fever Acid base derangements
Electrolyte abnormalities Nutrition: parenteral and enteral
Disseminated intravascular coagulation Hemolysis
Sedation Drug induced paralysis
Core Competencies addressed in this rotation
Patient Care
- Mastering surgical resuscitation.
- Experience with longitudinal care of the trauma patient
- Experience with the complications of severe fractures
- Experience with the complications of severe thorax injuries
- Experience with the complications of severe vascular injuries
- Experience with the complications of severe head injuries
- Experience with the complications of multi-organ dysfunction
- Post-operative care of the critical patient
- Ventilator Management
Medical Knowledge
- Learning and avoiding common errors in surgical critical care
- Gaining an understanding of the unique issues pertinent to surgical patients
- Gaining an understanding of the unique issues pertinent to post-op patients
- Pain control strategies
- Cognitive mastery of emergent trauma care
- Ventilator weaning protocols and procedures
Interpersonal and Communication Skills
- Working with surgical, trauma, orthopedic, nutrition, rehab, neurosurgical and medical professionals
- Working with respiratory, Social Services, PT ancillary services
- Integration into an ICU team with critical injuries
- Patient/family communication and comfort
Professionalism
- Integration into an surgical critical care team
- Pain Management
Systems-Based practice
- Integration into the ancillary services of Social Services, discharge planning, utilization review, OT and PT.
- Admission and transfer criteria for critical surgical patients
Practice Based Learning and Improvement
- Participate in CQI system of surgical department
- Participate in trauma/surgical M&M case conferences
- Maintain resident portfolio
Stroke
Meeting place: SUNY Downstate
Contact Number:
Daily Rounds: 7 AM
Responsibilities: Full participation in the Neurology service at UHB, including:
- Patient care under the direction of the Neurology Senior resident and Attending Staff
- Resident rounds at 7 AM Monday - Sunday
- Attending Neuro-Critical Care rounds 7:30 - 9 AM Monday to Friday
- Attending General Neurology rounds 9:30 – 12 N Monday – Friday
- Attending Rounds (all services) 9 AM weekends and holidays
- Neuroradiology rounds 11 AM on Mondays
- Neurology Grand Rounds 9 AM on Fridays
- Case conference 12 N on Fridays
- Participate in the resident call schedule (approximately 1:4)
EM Faculty Liaison: Dr. Mark Silverberg Cell: 917-822-4510
Neurology Faculty Liaison: Dr. Helen Valsamis Cell: 917-790-0446
Beeper: 917-760-0888
Educational Objectives:
PGY-2 Emergency Medicine Residents will rotate for two weeks on the Stroke service at UHB. They should be there at 7AM every day except for Wednesdays. On Wednesdays they are to show up for the regular EM conference at Kings County Hospital at 7 AM, but are expected to report to UHB Wednesday afternoon to resume usual duties. While rotating at UHB, residents will work under the direction of the Neurology Attending staff as part of the Neurology Stroke/Critical Care team.
Each day that the residents are at the UHB on the Neurology service, they should follow the Neurology Residents and Attendings in their daily rounds and consults. In addition, the EM resident will attend all Department of Neurology conferences and educational events.
At the completion of this rotation the resident will demonstrate competence in the following concepts:
- Performance of a comprehensive neurologic history and physical exam. (MK,PC)
- Development of an integrated problem list for patients, including detailed differential diagnoses. (MK,PC)
- Learn to localize neurological lesions in the CNS after performing a comprehensive neurological history and physical examination. (MK,PC)
- Management of stroke; ischemic and hemorrhagic. (MK,PC)
- Basic understanding of the principles of Neuro-critical Care (MK,PC)
- Evaluation and treatment of the Transient Ischemic Attack. (MK,PC)
- Basic Head CT and MRI interpretation. (MK,PC)
- Development of the Doctor-Patient relationship as the resident interacts with patients and their families during the stress of illness and death. (PC,C,P)
Description of clinical experiences:
Residents should demonstrate competence in the following procedures on this rotation:
Lumbar puncture
Description of didactic experiences:
The following topics should be covered in the resident’s reading during this rotation:
Cerebral aneurysm Arteriovenous malformation
Intracerebral hemorrhage Stroke etiology, evaluation, and management
Ischemic stroke Transient ischemic attack
Subarachnoid hemorrhage Bell’s palsy
Thrombolysis in Stroke Angiography and endovascular treatment in Stroke
Emergency Orthopedic/Fast Track Rotation
Orthopedics is a major component of the daily cases seen by Emergency Medicine physicians. The goal of this rotation is to increase orthopedic exposure to the emergency medicine residents so that they feel comfortable managing various orthopedic emergencies. The other goal of this Orthopedic / Fast Track Rotation is be able to evaluate and manage patients with all types of minor emergencies.
The rotation is 4 weeks spent in the fast track emergency department at Kings County Hospital. Two weeks will be spent on the Orthopedic Rotation and two weeks will be spent on the Fast Track Rotation. When there are 2 EM Residents or both an EM & an EM / IM Resident on this Rotation at the same time, the schedule will be made so that one resident will be on Ortho and one on the Fast Track Rotation, and then for the next two weeks the residents will “flip their assignments” with the Ortho Resident switching to the Fast Track Rotation, and the Fast Track Resident switching to the Ortho Rotation.
Please note that the PGY2 Categorical EM Residents will spend 4 weeks on the entire rotation. The PGY3 EM / IM Resident will also spend 4 weeks on the rotation, and will do both parts of the rotation.
1. The Ortho Part of the Rotation: The resident is to evaluate as many orthopedic emergency cases as possible that come through the emergency department. The resident will be based in the Fast Track Area. The residents are allowed to “cherry pick” orthopedic cases from the “White Board” of the Fast Track Area. If there are no traumatic orthopedic injuries on the “Board”, then the resident will see patients with non-traumatic musculo-skeletal complaints. If there are no orthopedic type cases at all in the Fast Track Area, then the resident will see cases that involve procedures, such as suturing and incising & draining abscesses. If there are none of any of the above type cases, then the resident will see “regular fast track cases”. When orthopedic cases are identified in Suite A and B, the Pediatric ED, CCT, or Fast track by other ED attendings or residents, the ED orthopedic resident will be paged to those areas to see these patients. There is an orthopedic pager – pick it up from Dr. Gernsheimer. The ED Orthopedic Resident should post his or her name and the Pager Number in all the ED areas at KCH. When paged to any of the ED areas, the ED Ortho Resident should go to that area. As noted above, if there are no orthopedic trauma cases (fractures/sprains), the resident should see musculo-skeletal cases. If there are no orthopedic or musculoskeletal cases the resident should see regular fast track cases, especially cases involving performing minor procedures.
Every orthopedic case and procedure must be placed in the residents’ personal logbook, a copy of which will be collected at the end of the rotation.
If the orthopedic case requires surgical intervention, admission, requires additional assistance or is beyond the scope or comfort of the Emergency Medicine attending, the orthopedic consult resident should be called. When able to, the ED orthopedic resident should be the one calling the orthopedic resident for the consult.
Emergency Medicine residents should also see pediatric orthopedic cases; however, the orthopedic resident should be called to see these cases as well.
On days when the emergency medicine resident is working during the day, the resident is to also go to morning orthopedic surgery resident rounds to go over the patients that were formally consulted the previous day. Be prepared.
The resident work schedule is usually the following:
Monday and Tuesday 6a-6p (Morning report is at 6am in C – 3 and you are required to be there)
Thursday and Friday 11a-11p (no morning report on these 2 days)
On Wednesdays the residents on the Ortho Rotation and on the Fast Track Rotation will attend the morning conferences and any other academic activities they are assigned to for that day, such as Board Review or Simulations, and then they will be free to read. The EM / IM residents assigned to Ortho will attend their Primary Care Clinics in the afternoon.
On the second Wednesday of the month from 2 PM – 4 PM, there is a Mid-Level Provider Conference held in our Main EM Conference Room and I am requiring the Categorical EM Residents to attend this conference.
Changes in the above schedule has to be approved by Dr. Jeffrey Levine, the Director of KCH Fast Track: e-mail: JTL8499@aol.com and Dr. Gernsheimer
Supervision: When working in the Fast Track Area, the EM Residents should be supervised by an EM Boarded Physician. When seeing Ortho patients in the other areas, the EM Residents should be supervised by an EM Boarded or PEM Attending.
Contact Dr. Gernsheimer prior to the start of your rotation –
gernsh@aol.com, cell – 917-750-1145, pager – 917-219-1976
Dr. Gernsheimer will supply you with important information regarding this rotation, a syllabus, a summary of this section from the Hand Book, the Ortho Patient Log, the Ortho Pager and a copy of the Emergency Orthopedic Text by Simon.
Orthopedic Examination Required Reading
- General Principles of Orthopedic Injuries (from Rosen’s) – You can access this online from our library.
- Ankle and Foot – (from Rosen’s). – you can access this online from our library
- Injury to the Hand and Digits – Tintinalli p1665-1674
- Wrist Injuries – Tintinalli p 1674-1684
- Injuries to the Shoulder Complex and Humerus – Tintinalli p1695-1702
- Knee Injuries – Tintinalli p1726-1734
- Leg Injuries – Tintinalli p1734-1736
- **** Emergency Orthopedics by Robert Simon. I will provide a copy for you to use while you are on the Ortho part of the rotation. It is also available online from our library. It is my favorite Emergency Ortho Text – JG
On the last Wed conference of the block (before you switch), the residents will have an Emergency Orthopedics examination. The exam will consist of multiple-choice questions and five essays. The essays will consist of interpretation of orthopedic x-rays, including injury complications, correct orthopedic fracture nomenclature and management of these various injuries. It should take ~1 hour to 1 ½ hours to complete the entire exam.
Part of your final examination in orthopedics will be to turn in your Orthopedic patient log to Dr. Gernsheimer. The log should include the cases that you have seen, the procedures that you did, and interesting x-rays.
2. The Fast Track Part of the Rotation: When on the Fast Track Part of the Rotation, the assigned resident will work in Fast Track and see Fast Track cases from the Fast Track “White Board”. They will not go to do consults in the other ED areas. Although, they will usually see Fast Track Patients in the order that the patients are on the “Board”, we would like them to try to do as many minor procedures as possible, and log these procedures in the usual manner on New Innovations. While on this part of the rotation, we want the resident to get very confident and competent in managing all types of minor emergencies.
Supervision: While on this part of the Rotation the EM Resident will be supervised by an EM Boarded Attending Physicians in the KCH Fast Track Area.
Schedule: The preliminary schedule will usually be:
Mondays: 7a – 7p
Tuesdays: 7a – 7p, so that the resident can attend conferences on Wednesday Morning starting at 8 am.
Wednesday – Morning Conferences from 8a – 12 noon, and then any academic activities that the resident has been assigned to. On the 2nd Wednesday of the month this resident will attend the Mid-Level Provider Conference from 2 PM – 4 PM.
Thursdays: 11 a – 11 p
Fridays: 11a – 11p
PLEASE NOTE: Dr. Levine may have to adjust this schedule to insure that the FT Resident is always with an Emergency Medicine Boarded Attending.
All Schedule Changes must be approved by Dr. Levine and Dr. Gernsheimer
Reading:
While on the Fast Track Portion of this rotation, the resident is expected to read on all the different types of cases that she or he sees.
References:
- Minor Emergencies by Philip Buttaravoli. Dr. Gernsheimer will supply you with a copy of this very practical text when you are on this part of the rotation.
- Tintinalli
- Rosen
- The procedure by Roberts and Hedges.
These 3 books are available on-line via the Downstate Library.
Any questions or problems regarding the Orthopedic / Fast Track Rotation should be addressed to Dr. Gernsheimer at the contact information listed above.
PGY-3 OFF SERVICE ROTATIONS
EMS
Toxicology
Ultrasound
Research
EMS
FDNY EMS RESIDENT / FELLOW ROTATION INFORMATION
The EMS rotation starts on the Monday morning of the first week of the 2-week block. Residents from Emergency Medicine Programs throughout New York City meet at 9am with one of the EMS Medical Directors at the Fire Department’s Headquarters, located at 9 MetroTech Center in Downtown Brooklyn (Office of Medical Affairs, 4th floor conference room).
Enter the building from the courtyard side (not the entrance on Flatbush Avenue). You will need a picture I.D. in order to get past the police checkpoint outside the building, and also to obtain a visitors’ pass once inside the building (it is useful to have your hospital I.D. with you in addition to your driver’s license). Once inside, you will need to pass through a metal detector and will not be allowed upstairs with any knives, weapons, explosives, etc. (so please leave any such items at home as there aren’t any lockers or places for storage).
The morning of the first day includes a series of lectures and discussions about EMS and Disaster Preparedness in New York City as well as various academic EMS-related topics. The schedule and requirements for the rest of the rotation will be reviewed at that time. Usually there is a lunch break followed by some more discussions and a visit to the 911-Communications Center. The day is over by 4pm.
Each Resident will be given an individualized schedule for the 2-week block. Most days will require ride-alongs with an ambulance or EMS Supervisor. One of the days will be an observation at the On-Line Medical Control Facility (“Telemetry”) and there may also be a day assigned to teaching or testing EMT’s or Paramedics at our training academy. Most observations or ride-alongs are 8-hours long (e.g., 8am-4pm, 10am-6pm, 3pm-11pm). Weekends are usually left unscheduled, but may be used for rotation assignments. You will be required to be signed in and out each day.
Due to the unique structure of this rotation, attendance at, and arrival on time to, the first day of rotation is mandatory. Those who are absent or late will not be permitted to continue and will be requested to reschedule their EMS rotation.
The ride-alongs offer an opportunity for you to observe the capabilities of EMS providers and to give you insight into the care provided to patients prior to their arrival at the Emergency Department. The pre-hospital environment is less controlled than the Emergency Department, and therefore you must always be cognizant of scene safety and the potential for unsuspected situations to arise. The EMT’s and Paramedics are acutely aware of such things, and we always advise participants to stay close by your assigned providers at all times.
You will find the EMT’s and Paramedics are eager to involve you in the assessment and care of patients in order that they may gleam some of your medical knowledge and skills. However, your role on the ride-alongs is officially as an observer only.
There will be a few assignments for you to complete during the rotation. The assignments often include a write-up of an interesting patient you encountered during the ride-alongs or a simple research project on an assigned EMS topic.
PLEASE DISTRIBUTE TO ROTATING RESIDENTS IN ADVANCE OF ROTATION
On the Friday of the second week everybody again meets at the Fire Department Headquarters (or another predetermined location) to discuss the rotation, present the assigned topics, as well as review some other EMS issues. Your attendance as well as performance on the assigned topics helps determine your grade for the rotation.
It has been long agreed with the Residency and Fellowship Program Directors that, in return for leaving both Wednesdays during the rotation free for EM residency weekly conferences, the EMS rotating residents and fellows will not be scheduled for additional duties (e.g., ED shifts, Sick-Call, Back-Up, etc.) during this important short rotation. Those who miss EMS rotation assignments for such coverage will be dropped from the rotation. We have insisted that this constraint includes both rotation weekends in-order to allow for flexibility to accommodate for unexpected circumstances that may necessitate participants to complete their required tasks during these weekends.
All missed rotation days (for reasons other than the above) that were not completed during the rotation weekends, must be made up within four weeks. Until such time that the deficiency is corrected, a grade of ‘Incomplete’ will be issued. Beyond that point (four weeks), the incomplete rotation will become a rotation Failure.
ATTIRE: The first and last days of the rotation will be at the FDNY Headquarters building. As this is an office environment, you will be expected to dress accordingly (pants/skirt,
shirt/blouse, tie, shoes). The only exception is that if you have worked Sunday overnight in the ED prior to the first-day Monday session, scrubs will be permitted. When riding-along on an ambulance, you will be expected to wear dark pants and a work shirt (e.g., long-sleeve button- down). It is especially important to wear closed shoes that are comfortable to do a lot of walking in. Please do not wear jeans, t-shirts, scrubs, sneakers, or sandals on the ride-alongs. Of course, always carry hospital identification visibly on your outermost garment at all times.
EMS RESIDENCY ELECTIVE: Some Residents have a greater interest in the Medical Direction of EMS, and may in fact desire to do a Fellowship and receive subspecialty Board
Certification in EMS. For such individuals, FDNY offers a two to four week senior-resident Advanced EMS Elective. This experience offers the opportunity to learn about EMS Medical Direction by participating with the FDNY Medical Directors in meetings, operational activities, exercises, research, and all aspects of a Medical Director’s responsibilities. Additionally, we welcome Residents who are interested in working on EMS research (either joining an ongoing project or developing a new one).
CONTACT INFORMATION: For questions or additional information, please feel free to contact:
• €Ms. Pekoia Jenkins EMS Resident Rotation Program Coordinator (jenkinp@fdny.nyc.gov,
718-999-1227)
• €David Ben-Eli, MD, EMS Resident Rotation Program Director (benelid@fdny.nyc.gov, 718-
999-2790)
• €Douglas Isaacs, MD, EMS Fellowship Program Director (isaacsd@fdny.nyc.gov, 718-999-
2790)
Dear Program Director / Coordinator,
4/12/2013
Attached are the EMS rotation dates for the upcoming academic year 2013‐2014. This is to be used to schedule your residents for rotations through the New York City Fire Department Emergency Medical Services (EMS).
As in last year, we will be offering a total of fourteen two‐week rotation blocks. With the expected rise in the number of participants, we have increased the number of available slots per rotation block to 12. The assignments will be based on a first‐come basis. Therefore, please email your requests to our EMS Rotation Program Coordinator, Ms. Pekoia Jenkins (jenkinp@fdny.nyc.gov), at your earliest convenience.
The structure of the two‐week EMS rotation remains unchanged from last year, and is as follows:
•Meeting at FDNY Headquarters, introduction to EMS and Disaster Preparedness, tour of FDNY Command and Dispatch centers, Disaster Preparedness tabletop exercise, rotation assignments discussion ‐ first day (usually
Monday)
•Supervisor ride‐along – two days
•On‐Line Medical Control experience ‐ one day
•ALS ride‐along ‐ two days
•BLS ride‐along ‐ one day
•Meeting at FDNY Headquarters, discussion of cases experienced during rotation (ambulance ride‐alongs,
Telemetry), and research topic / project presentations ‐ last day (usually Friday)
•Both Wednesdays during the rotation are kept free for EM residency weekly conferences.
Following are a number of ground‐rules to ensure a smooth EMS rotation academic year. Your cooperation is greatly appreciated:
1. Unless otherwise directed, the first and last days of each rotation block will be conducted at the FDNY Headquarters, 9 MetroTech Center, Brooklyn, in the 4W‐6 conference room. We have attached directions as well as a brief introduction to the rotation. Please be sure to distribute these to your rotating residents / fellows prior to their assigned rotation start date.
2.Please note that the participants will be required to pass through two security check‐points prior to being permitted to enter the FDNY Headquarters on the first and last days of the rotation. Security must be provided well in advance with the list of participants scheduled to arrive for each EMS rotation. Therefore, it is imperative that you provide a schedule with the accurate names of your residents / fellows according to date‐of‐ participation, in‐order to prepare this list for Security. In‐accuracies will prevent the participants from entering the building, and they will be dropped from the rotation.
3. Due to the unique structure of this rotation (as outlined above), attendance at, and arrival on time to, the first and last days of the rotation is mandatory. Those who are absent or late will not be permitted to continue and will be requested to reschedule their EMS rotation.
4. The role of participants on the ambulance ride‐alongs is officially as observers only. They are not permitted to engage in any patient‐care activity, including, but not limited to, patient‐assessment, procedures, and provision of Medical Control (as well as securing Refusal of Medical Aid and transport decisions).
5. Participants should be reminded that business attire (shirt / blouse, tie ‐ no scrubs, jeans, sneakers, Crocks, etc.) is expected during the EMS rotation with the Fire Department, and that they must carry hospital‐identification visibly on their outermost garment at all times.
6. Scheduling EMS rotations and ambulance ride‐alongs for most of New York City’s Emergency Medicine residents and fellows is a very long and tedious process, complicated by having to coordinate the participants’ activities with other groups (e.g., EMT and Paramedic students, Armed‐Forces and government personnel, etc.), resulting in little‐to‐no flexibility for schedule changes and last‐minute requests. We thank you for your understanding!
7. It has been long agreed with the Residency and Fellowship Program Directors that, in return for leaving both Wednesdays during the rotation free for EM residency weekly conferences, the EMS rotating residents and fellows will not be scheduled for additional duties (e.g., ED shifts, Sick‐Call, Back‐Up, etc.) during this important short rotation. Those who miss EMS rotation assignments for such coverage will be dropped from the rotation. We have insisted that this constraint will include both rotation weekends in‐order to permit flexibility for accommodating unexpected circumstances that may necessitate participants to complete their required activities during these weekends.
8. All missed rotation days (for reasons other than the above) that were not completed during the rotation weekends, must be made up within four weeks. Until such time that the deficiency is corrected, a grade of ‘incomplete’ will be issued. Beyond that point (4 weeks), the incomplete rotation will become a rotation failure.
Educational Objectives:
The EMS rotation will provide a general exposure to the medical, regulatory, legislative, administrative, political, and organizational aspects of pre-hospital care. By completion of this rotation, the resident will have developed the basic groundwork for understanding the structure and function of Emergency Medical Services. The resident will spend two weeks on this rotation. The base for the rotation will be the FDNY EMS Service. The Emergency Medicine Resident will accompany EMTs and Paramedics on ambulance runs. This will be supplemented with experience working side by side with the EMS medical director in performing all tasks of the medical director. Residents will conduct Paramedic and EMT training in the form of call review and formal lectures. The FDNY medical director will evaluate performance based on competence, understanding and enthusiasm for the required activities. Much of this rotation will be self-directed learning. A list of readings appropriate to the rotation will be provided.
At the completion of this rotation the Resident will demonstrate competence in the following concepts:
• The history and development of EMS(MK)
• The political forces which impact on EMS(SBP)
• Hospital and departmental categorization(SBP)
• The principles of disaster management and preparedness(MK)
• The training of prehospital personnel(C,P)
• The role of the Emergency Physician and Department in the training of pre-hospital personnel(P,C,PBL)
• The contributions of the various participants in an EMS system(MK,P,C)
• The various organizational structures of EMS systems(MK,SBP)
• The concepts of medical control(MK,SBP)
• The various EMS protocols and their applications(MK,SBP)
• The principles of EMS communication and 911(MK,SBP,C)
• Fiscal and regulatory issues related to EMS(MK,SBP)
Description of clinical experiences(MK,PC)
Residents should have experience and demonstrate competence in the following procedures on this rotation:
• Assessing scene safety
• Functioning as off-line medical control
• Providing medical care in the pre-hospital environment; including procedures as:
• Extrication
• Immobilizations and spine injury precautions
• Airway management in the field
• Vascular access in the field
Description of didactic experiences: (MK,PC,SBP)
The following topics should be covered in lectures or readings during this rotation:
A. Overview
1. History of EMS
2. National, state, and local
3. Various types of service
4. Level of care
5. Volunteer vs. hospital based vs. city/county based vs. commercial
B. Fiscal Aspects of EMS
1. Costs and resources, billing
C. Organizational Aspects of EMS
1. Levels of EMT training and skills; fire, police, MD, administrators
2. Equipment and vehicles
3. Local, state, and federal regulations
4. EMS Medical Director
5. Development of 911
6. Receiving and dispatch
7. Communications and telemetry systems
8. Field triage
9. Interface with other services (police and fire)
D. Categorization and designation of hospitals and hospital services
E. Medical Control
1. Centralized vs. decentralized
2. The role of the Medical Director
3. The role of the Emergency Physician
4. Development and implementation of protocols
5. On-line and off-line medical control
6. Call review and CME for the prehospital provider
F. Air Transport Systems
G. Disaster Planning and Management
1. Planning for prehospital disasters
a. The EMS role
b. The hospital role
2. Special disasters
a. Biological
b. Chemical
c. Radiation
H. Education
1. CPR
2. EMT
3. AEMT
4. EMT-P
5. First aid and first responder training
6. Public education
I. The Role of EMS in Public Education
1. Issues of organization
2. Issues of medical treatment and level of care
TOXICOLOGY
EM Faculty Liaison: Dr. Sage Wiener
Description and Goals of Rotation: The rotation at the New York Poison Control Center (NYCPCC) is your opportunity to exclusively focus on medical toxicology. During the rotation you should make an effort to become familiar with general approaches to the poisoned patient and clinical presentations of common toxidromes. You should also develop a basic understanding of poison prevention techniques, pharmacokinetics, toxicokinetics, resuscitation of the poisoned patient and commonly used antidotes.
Meeting Place: 8:15 AM in the Bellevue Hospital Emergency Department conference room for morning report. After morning report, residents should go to the New York City Department of Health/NYCPCC ground floor conference room. The address is 455 1st Avenue (corner of 26th Street). Check in with one of the toxicology fellows upon arrival.
NYU/Bellevue Hospital Center
New York City Poison Control Center
Schedule: Weekdays: 8:15 AM - 4:00 PM
Contact: Dr. Lewis Nelson, Director, Fellowship in Medical Toxicology
Tel: (212) 447-8150
Special Considerations:
1. Attendance at the Bellevue Department of Emergency Medicine Morning Report is mandatory.
2. The morning will be spent doing follow-up calls and the afternoon generally is dedicated to didactic teaching rounds.
3. All residents rotating at the poison center are required to present a topic (project) that interests them by the end of their rotation. When deciding on a presentation topic, , discussion with one of the toxicology fellows is imperative so that you may be properly focused. The talk should be designed to educate the group (toxicology attendings, fellows, residents and medical students) and attempt to answer a question that has been raised regarding a specific clinical case. The talk should be at most 10 minutes in length. A handout may be helpful but a formal PowerPoint slide presentation is excessive.
4. Once a month, there will be a Consultants’ Conference meeting scheduled on the first Thursday at 2:00 PM. It is usually held in the ground floor auditorium of the Department of Health building where the poison control center is located. You are welcome to continue going to these conferences during other blocks if you are free. This is an especially good idea if you are considering applying for a toxicology fellowship.
5. Take advantage of your time at the NYCPCC as other physicians from all over the United States and other countries come to New York City to participate in the elective. This is not the month to “blow off” days. Be on time and actively participate in toxicology rounds.
6. Residents are required to attend weekly KCH Wednesday Emergency Medicine Departmental Conference
RESEARCH
Active participation in a research project is a requirement for all residents in the Department of Emergency Medicine. Residents will receive a two-week period during the second year of residency and a two-week period during the third year of residency dedicated to their research projects. These research periods will be assigned during an Emergency Department rotation at Kings County. In order for this time to be productive, it is extremely helpful to have a project planned before you begin the initial two-week period. The resources necessary to successfully complete your project, including statistical and administrative support will be provided by the department.
Attendance at Wednesday conference is mandatory.
If the resident does not contact the research division at least 4 weeks prior to beginning the research rotation, the resident will be scheduled for shifts in the ED.
One Thursday at 11am during the month, the resident will participate in a combined Emergency Medicine/Trauma Service simulation session in the simulation lab. Contact the simulator division for further information the month prior to the start of the rotation.
How to Start?
On the first Wednesday of every month, ongoing projects are reviewed and new research projects are presented during conference. This information is available on the ED website in the Research Update newsletter. The Research Update is also posted monthly on the research bulletin board outside of the conference room. All PGY II and III residents should contact Dr. Zehtabchi (shahriar.zehtabchi@downstate.edu) at least one month prior to the start of their research rotation to setup a project. Residents are strongly encouraged to start a new project, starting from literature search, study design, planning the logistic aspects of the project, etc. However, they may join projects already in development, and completing or helping to complete a research project of suitable quality for publication may fulfill the requirement. For authorship in a manuscript, residents need to meet the criteria outlined in the authorship policy that is published in the monthly research update.
IRB Certification:
All attendings and residents are required to obtain the certification for “Human Participants Protection Education.” To complete your certification, please sign on to CITI (Collaborative IRB Training Initiative) computer based training program at http://www.miami.edu/bb/sunyreg.
Didactic Research Lectures:
The first Wednesday of each month, the research division will have a one hour lecture dedicated to research methodology, biostatistics, and evidenced-based medicine. All residents and faculty are welcome to attend these lectures. The topics of these lectures are published at the beginning of each year in the annual research update handbook.
Research Office Hours:
Every Wednesday Dr. Sinert and Dr. Zehtabchi will be available in their offices (9 am to 4 pm) to meet with faculty and residents on research issues. Please contact them one week in advance to set up a time.
How to Choose a Project:
The department of emergency medicine offers the residents research projects in a variety of emergency medicine fields. Residents are welcomed to start their own projects or to join the investigators of one of the active projects. The faculty and residents of the department of emergency medicine have conducted several research projects in the field of Trauma and Hemorrhagic Shock, Sickle cell Anemia, Toxicology, Evidenced-Based Medicine, and Medical Student/Resident Education.
Academic Associates Program:
The Academic Associate Emergency Medicine Clinical Research Program teaches the fundamentals of research to undergraduate pre-med students and medical students. This course is modeled after the novel clinical research elective Dr. Hollander first developed at SUNY Stony Brook. The Academic Associates work in conjunction with the ED staff to help identify and enroll patients who meet the specific inclusion/exclusion criteria for our clinical trials. The Academic Associates are responsible for the appropriate paperwork and data processing within the required time frame for each of the studies. Duties include data collection, collation, forms processing, and assisting in database configuration, statistical analysis, and abstract and manuscript preparation. Coupled with the “hands-on” data collection, a didactic program focusing on research design, and basic statistics will be organized for the academic associates by the research division. This program stresses professional responsibility, independent thinking, research design and data collection methods. Non-medical student Academic Associates (college students) are not permitted to draw blood, or handle laboratory specimens. Please remember that they are college students with no formal medical training.
Please make them feel at home and do not hesitate to help them perform their tasks in any way you can.
Policy: Authorship and Contributorship
Byline Authors
An "author" is generally considered to be someone who has made substantive intellectual contributions to a published study, and biomedical authorship continues to have important academic, social, and financial implications. (1) In the past, readers were rarely provided with information about contributions to studies from those listed as authors and in acknowledgments. (2) Some journals now request and publish information about the contributions of each person named as having participated in a submitted study, at least for original research. Editors are strongly encouraged to develop and implement a contributorship policy, as well as a policy on identifying who is responsible for the integrity of the work as a whole.
While contributorship and guarantorship policies obviously remove much of the ambiguity surrounding contributions, it leaves unresolved the question of the quantity and quality of contribution that qualify for authorship. The International Committee of Medical Journal Editors has recommended the following criteria for authorship; these criteria are still appropriate for those journals that distinguish authors from other contributors.
• Authorship credit should be based on 1) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; 2) drafting the article or revising it critically for important intellectual content; and 3) final approval of the version to be published. Authors should meet conditions 1, 2, and 3.
• When a large, multi-center group has conducted the work, the group should identify the individuals who accept direct responsibility for the manuscript (3). These individuals should fully meet the criteria for authorship defined above and editors will ask these individuals to complete journal-specific author and conflict of interest disclosure forms. When submitting a group author manuscript, the corresponding author should clearly indicate the preferred citation and should clearly identify all individual authors as well as the group name. Journals will generally list other members of the group in the acknowledgments. The National Library of Medicine indexes the group name and the names of individuals the group has identified as being directly responsible for the manuscript.
• Acquisition of funding, collection of data, or general supervision of the research group, alone, does not justify authorship.
• All persons designated as authors should qualify for authorship, and all those who qualify should be listed.
• Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Some journals now also request that one or more authors, referred to as "guarantors," be identified as the persons who take responsibility for the integrity of the work as a whole, from inception to published article, and publish that information.
Increasingly, authorship of multi-center trials is attributed to a group. All members of the group who are named as authors should fully meet the above criteria for authorship.
The order of authorship on the byline should be a joint decision of the co-authors. Authors should be prepared to explain the order in which authors are listed. .
For further information on this and other policies visit http://www.icmje.org.
Research Contact Numbers:
Dr. Richard Sinert:
Director of Research
Telephone extension 2973
E-mail: nephron1@gmail.com
Dr. Shahriar Zehtabchi
Associate Director of Research
E-mail: shahriar.zehtabchi@downstate.edu
Dr. Lorenzo Paladino
Assistant Director of Research
Beeper: (917) 219-6276
lorenzopaladino@yahoo.com
Dr. Richard Shin
richard.d.shin@gmail.com
Chief Resident of Research
Name:
Department of Emergency Medicine
Scholarly Project Completion Form
All residents are required to complete a scholarly project during their residency.
This project must be found satisfactory by the Program Director or his/her designee.
Title of Project:
Description: ______________________________________________________________________________________________________ _____________________________________________________________________________________________
Faculty or Mentor Comments: _________________________________________________________________________
Project Completed Date: ¬¬¬¬¬¬¬¬¬¬¬¬¬¬¬¬¬¬_______________________________
Was this project of publishable quality: Yes No
Was this project published: Yes No
If so, where: __________________________________________________________
Congratulations on your successful completion of the Scholarly Project.
____________________________________
Resident Signature
____________________________________
Faculty Mentor Signature
____________________________________
Residency Director Signature
EMERGENCY ULTRASOUND ROTATION
TRAINING LEVEL: PGY 3 AND/OR PGY 4
DURATION: 4 WEEKS (2 WEEKS as PGY-3 and 2 WEEKS AS PGY-4)
LOCATION: UHB and KCH ED
FACULTY LIASON:
Dr. Schechter Cell: (646) 281-1136
Email: joshschecht@gmail.com
FACULTY:
Dr. Secko Cell: (631) 645-7200
Email: michael.secko@downstate.edu
Dr. Mehta Cell: (917) 642-6139
Email: ninfa.mehta@gmail.com
Dr. Liz Rubano Cell: 646-261-1395
Email: elrubano@gmail.com
Dr. Theresa Smith Cell: 347-768-2933
Email: teresaemergencymd@gmail.com
Dr. Papanagnou Cell: (917) 596-3828
Email: erdocny@gmail.com
Dr. Gleyzer Pager: (917) 761-1098
Email: gleyzer1@gmail.com
Dr. Kelly Maurelus Email: maurek01@gmail.com
FELLOWS 2013-2014:
Dr. Andrew Aherne Email: andrew.aherne@gmail.com
Dr. John Kilpatrick Email: jfk.emergency@gmail.com
OBJECTIVES:
1. To understand basic physics and instrumentation of medical ultrasound equipment
2. To learn how to use the ultrasound systems available in KCH and UHB Emergency Departments
3. To review normal sonographic anatomy and pathophysiology of the thorax, abdomen and pelvis.
4. To understand indications and limitations of bedside emergency ultrasound.
5. To learn how to perform the following studies:
a. Extended Focused Assessment with Sonography in Trauma (E-FAST)
i. Hemoperitoneum
ii. Hemopericardium
iii. Hemothorax
iv. Pneumothorax
b. Focused Gynecologic and Obstetric Ultrasound
i. Intrauterine pregnancy
ii. Ectopic pregnancy
iii. Threatened/Incomplete/Complete Abortion
iv. Ovarian cysts/adnexal masses
c. Focused Biliary Ultrasound
i. Gallstones
ii. Cholecystitis
iii. Choledocholithiasis
d. Focused Echocardiography
i. Pericardial effusion
ii. LV and RV function
iii. Gross valvular abnormalities
iv. Volume assessment
e. Focused Abdominal Aorta Ultrasound
i. Aortic aneurysm
ii. Aortic dissection
f. Focused Renal Ultrasound
i. Hydronephrosis
ii. Urolithiasis
g. Focused Vascular Ultrasound
i. Deep venous thrombosis
h. Focused Skin and Soft Tissue Ultrasound
i. Abscess
ii. Foreign body
iii. Cellulitis
iv. Tendon injuries
v. Fractures
vi. Dislocations
i. Focused Ophthalmic Ultrasound
i. Retinal detachment
ii. Vitreous hemorrhage
iii. Lens dislocation
iv. CRAO/CRVO
j. Ultrasound guided vascular access and additional US guided procedures
k. Regional anesthesia and musculoskeletal US
ATTENDANCE AND SCHEDULE: YOU MUST E-MAIL DR. SCHECHTER AT LEAST ONE WEEK PRIOR TO THE START OF YOUR ROTATION SO WE CAN ADJUST OUR SCHEDULES TO MEET WITH YOU
During the rotation the resident is expected to be present in the Department Monday – Friday 9am – 4 pm. Attendance is mandatory. Specific daily tasks will be assigned by the individual Attending of the day. On the first day of the rotation the resident is to report to the Kings County Emergency Department Offices to meet with Ultrasound Faculty and/or Fellows for orientation at 0900AM. Attendance at Wednesday Conference is mandatory. The residents must also meet on Thursdays at 9am for tape review located in US room next to the simulation center.
DIDACTIC TRAINING: Before starting the rotation, make sure you obtain a copy of the Guide to the Senior Resident Rotation for specific instructions on the use of the machines and an introduction to Emergency Ultrasound and the Ultrasound Curriculum
In the beginning of the rotation the resident will be assigned specific readings including articles and chapters from several textbooks. Articles will be provided. All textbooks are available at the Downstate Medical Library and in on-line format. Ultrasound Journal Club will be conducted during the second week of the rotation and residents are required to briefly discuss a paper from the recent literature relevant to Emergency Ultrasound. Each resident must be prepared to present one ultrasound paper at tape review.
Required Scans: You will be required to fulfill a certain number of scans during your rotations.
Echo – 25
FAST – 20
Gallbladder – 15
Renal – 15
Lung – 15
DVT – 10
Aorta – 10
Ocular – 5
PRE-TEST: Must be taken prior to the start of the rotation.
You will given a pretest on the first day of your rotation. This is designed to help guide your education and areas that need improvement.
CLINICAL TRAINING:
During the rotation, a resident will be assigned to perform the following tasks:
1. Bedside US imaging under direct attending supervision
2. Bedside US-guided procedures under direct attending supervision
3. Independent bedside US imaging with weekly image review by division faculty
4. Responding to trauma codes for bedside e-FAST exams
5. Daily machine checks, machine maintenance and restocking of supplies
6. Enrollment of patients into active ultrasound research trials
7. Instruction of co-residents, interns and students
ACEP Quizzes: Throughout the rotation you will be required to take online quizzes in various topics depending on PGY year.
WEBSITE: www.emsono.com/acep
PLease
PGY-3:
• Physics
• Cardiac
• Biliary
• FAST (Trauma)
• GU (Renal and scrotal)
PGY-4:
• Physics
• DVT
• GU
• Ocular
• Soft Tissue
POST TEST: Must be taken at the end of the rotation
A test will be administered on the final Thursday of the block. You will receive by e-mail you score and any areas that need improvement.
EVALUATION:
Upon completion of the rotation, the resident will be evaluated based on his/her attendance, motivation, didactic knowledge, procedural skills, and test results. The evaluation form will be submitted to the residency directors and will be placed in the resident’s file. The resident will have access to the evaluation. The resident will be also asked to evaluate the rotation and provide suggestions on its improvement.
PRIOR TO STARTING THE ROTATION GO TO: http://www.sunysono.com
Then click on "Resources", and then click on the Guide to Senior Rotation.
Note:
1. Currently at UHB all studies are stored to the internal hard drive on the Philips HD11XE and MTurbo. At KCHC all studies are stored to the internal hard drives of the SonoSite MTurbo (there are 3) and GE LogicQ P5 systems. The Division faculty and fellows will orient you to image documentation on the first day of the rotation.
2. Image interpretation. ALL STUDIES WITHOUT EXCEPTION MUST CONTAIN THE FOLLOWING:
a. Sonographers’ last name(s)
b. Patient’s MR number
c. Interpretation in text on the screen (i.e. RUQ, no FF)
3. Do NOT log your studies into any procedures database. The Ultrasound Division keeps an independent record of your ultrasounds for credentialing and QA purposes.
PGY-4 OFF SERVICE ROTATIONS
Free Elective:
Medico-legal
Medical Examiner
Dermatology
Oral Surgery
Others
Administration
ELECTIVE
EM Faculty Liaison: Dr. Stephan Rinnert
The elective rotation is an opportunity for residents in their final years of training to gain experience in an aspect of Emergency Medicine that is not part of our formal residency curriculum or in-depth study of a field of EM. In very general terms, the goal of the rotation is for the resident to strengthen an area of clinical weakness or to learn more about one of the subspecialty areas of Emergency Medicine.
You are responsible for setting up your own elective.
Rotations away from SUNY Downstate are acceptable (for now) but require planning on your part.
Any elective away from Downstate needs to be applied for at least three months in advance. You need to obtain an Away Elective Planner/ Worksheet from The residency coordinator
Possibilities for outside rotations include Hyperbarics, Radiology, Burn Unit, Ultrasound training, International Emergency Medicine (Brazil, South Africa, Lesotho, Mexico, Nepal, Sweden, Haiti, Malawi, Botswana, Jamaica, Turkey, Romania and others), Research, Rural Emergency Medicine, Sonography, EMS, Pediatrics, or Toxicology and many others.
Creativity in planning your rotation is encouraged, but you must develop an education plan for the rotation. The Program Director will want to see your Goals and Objectives for the rotation, so plan them and put them in the elective planner. All rotations need to be approved by Dr. Rinnert before arrangements are made with an outside institution. At least 28 days before the rotation, please review your educational plan with Dr. Rinnert and fill out the elective planner (available from Stephanie Lane and below). If you buy plane tickets or make travel plans without having an approved elective, then YOU HAVE MADE A GRAVE ERROR.
If you are going to do an international elective, then you need to fill out an international elective planner IN ADDITION TO the standard elective planner. See the next section for the international elective planner.
If you are going to work in a clinical area, malpractice insurance coverage may be an issue. Your standard residency malpractice coverage only applies to resident activities, and your coverage will apply only to SUNY, its affiliates, and HHC hospitals. It is also possible to apply for SUNY to cover/provide malpractice coverage and have SUNY cover your elective. This takes time to set up, so start early ( at least three months in advance). You can apply with the form below. Dr. Rinnert does not make the decision to provide this coverage, but will help you set up the elective. Attached is a simple form to be completed while planning your rotation. Finally, upon returning to SUNY Downstate, you will need a letter certifying proof of the rotation, and to submit a short written synopsis of the rotation or prepare a brief oral presentation.
Please Note:
Omission or Failure to adequately plan your Elective as outlined above in the appropriate time frame will result in irrevocable loss of your Elective time. You will be scheduled for clinical shifts instead. Please comply with this rule.
No Exceptions!!!!
ELECTIVE PLANNER WORKSHEET
Elective Planner
Name: Dates of elective:
Elective site:
Subject of elective:
The goal for the elective:
Briefly below or on attached sheet outline your plan for the elective (please include goals/objectives/evaluation methods for the rotation):
International Elective Curriculum
One year ahead
1. Pick a place (general; or specific if you already know it)
a. Consult the SUNY/KCH international elective database
b. Talk to your contacts/make new contacts through networking
c. Talk to departmental faculty
d. Ask Dr. Bloem
2. Define your learning objectives
3. Consider doing a project (or part of one)
4. Plan your budget and look for funding if needed
a. Consult the SUNY/KCH international elective database
6 months ahead
5. Plan a meeting to discuss your elective plan with Dr. Bloem
6. Submit your Elective Plan sheet
By one month after the completion of your elective
7. Submit your reflective statement addressing your experience and how you met your learning objectives, as well as at least one suggested way to positively impact the health system (emergency or otherwise) of the place where you worked. Please make sure to fill out the accommodations, budget, and contact information section for the sake of future rotators and projects.
International Elective Plan
Date: __________________________
Name of resident: ___________________________________________________
Location of planned international elective: _______________________________
Elective Point-Of-Contact Person and Title: ______________________________
Contact Address: ___________________________________________________
Contact Phone: _____________________________________________________
Second Elective Point-Of-Contact Person and Title: ________________________
Contact Address: ____________________________________________________
Contact Phone: _____________________________________________________
Accommodation Type (aka, house, apt, dorm): ____________________________
Address: __________________________________________________________
Phone: ____________________________________________________________
ESTIMATED BUDGET
Travel cost: ________________________________________________________
Accommodation cost: ________________________________________________
Food/daily expenses cost: _____________________________________________
Learning Objectives
Please describe below your objectives for your international elective. Include what you hope to learn, how many hours you plan to work, what activities you will be involved with, and whether this elective will be related to an International Division project.
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
Reflective Statement
Please describe in at 1-2 pages what your experience abroad was like. Include what your responsibilities were, what kind of activities you participated in, how their system and patient population differed. State how you met or were unable to meet your learning objectives (as per your Elective Plan).
Please list at least one suggested way to positively impact the health system (emergency or otherwise) of the place where you worked. If you have an idea for a project for the International Division (great!), please describe it here briefly.
Please make sure to fill out the accommodations, budget, and contact information section below for the sake of future rotators and projects.
Resident name: _____________________________________________________
Location of international elective: ______________________________________
Point-Of-Contact Person and Title: _____________________________________
Contact Address: ___________________________________________________
Contact Phone: _____________________________________________________
Second Point-Of-Contact Person and Title: _______________________________
Contact Address: ____________________________________________________
Contact Phone: _____________________________________________________
Accommodation Type (aka, house, apt, dorm): ____________________________
Address: __________________________________________________________
Phone: ____________________________________________________________
EXPENSES
Travel cost: ________________________________________________________
Accommodation cost: ________________________________________________
Food/daily expenses cost: _____________________________________________
Other expenses (please describe): _______________________________________
__________________________________________________________________
__________________________________________________________________
__________________________________________________________________
MEDICO-LEGAL
Location: Offices of McAloon & Friedman, P.C.
Contact: Offices of McAloon & Friedman
123 Williams Street, New York, NY
212-732-8700
Contact person: Wayne Roth
Description of Rotation:
The resident will spend a 2 or a 4 week block with at McAloon and Friedman, the law firm which represents HHC hospitals in most large malpractice cases. Work schedule is 5 days per week, Monday through Friday, excluding Wednesday morning.
Daily activities generally begin by 9:00am every morning, with residents acting as medical experts for selected cases. Attendance at Wednesday Conference is mandatory. The resident will work under the supervision of staff at McAloon & Friedman.
Goals and Objectives:
The resident will demonstrate competence in:
1. Definition and components of malpractice
2. Process of discovery
3. Review of the medical record from medico-legal perspective
4. Use of expert witnesses
5. Witness preparation
6. Deposition process
7. National Practitioner Data Bank
8. Risk management and reduction
9. Medico-legal issues revolving around consent and refusal of care
Evaluation:
At the end of the block, an evaluation form will be filled out by the supervising staff member at McAloon & Friedman. The resident will also fill out and submit a rotation evaluation form.
MEDICAL EXAMINER
Location: Office of the Medical Examiner
Contact: Medical examiner
718-221-0600 (ext. 214)
The resident will spend a 2-week block with the Office of the Medical Examiner. Work schedule is 5 days per week, Monday through Friday, excluding Wednesday morning. On Wednesday morning the resident will be expected to attend the ED weekly conference. The resident will work under the supervision of attending pathologist from the Office of the Medical Examiner.
Goals and Objectives:
The resident will demonstrate competence in:
1. Strategies for work-up of cases
2. Communication with police, district attorneys and other clinicians
3. Clinical emergency department correlations with actual autopsy findings
4. Process of death certification
5. Greater insight into the workings of the medical-legal system
Evaluation:
At the end of the block, an evaluation form will be filled out by the supervising staff. The resident will also fill out and submit a rotation evaluation form.
DERMATOLOGY
Location: KCHC & SUNY – Downstate Medical Center
Contact: Alan Shalita, M.D., Chairman , Dept. of Dermatology
718-270-1229
Description of Rotation:
The resident will spend a 2-week block with the Department of Dermatology. Work schedule is 5 days per week, Monday through Friday, excluding Wednesday morning. On Wednesday morning the resident will be expected to attend the ED weekly conference. The resident will work under the supervision of attending or senior residents from the Department of Dermatology.
Goals and Objectives:
The resident will demonstrate competence in the evaluation and treatment of:
1. Cancers of the skin
2. Dermatitis, including but not limited to:
Atopic
Contact
Eczema
Psoriasis
Seborrhea
9. Infections, including but not limited to:
Bacterial
Fungal
Parasitic
Viral
10. Maculopapular lesions, including but not limited to:
Erythema multiforme
Erythema nodosum
Henoch-Schonlein purpura (HSP)
Pytiriasis rosea
Purpura
Urticaria
11. Papular/Nodular lesions, including but not limited to:
Hemangioma/Lymphangioma
Lipoma
12. Vesicular/Bullous lesions, including but not limited to:
Pemphigus
Staphylococcal scalded skin syndrome
Stevens Johnson syndrome
Toxic epidermal necrolysis
ORAL SURGERY
Location: KCHC & SUNY – Downstate Medical Center
Contact: Stewart K. Lazow, M.D.
718-245-2987
917-253-0002 (pager)
Description of Rotation:
The resident will spend a 2-week block with the Department of Oral Surgery. Work schedule is 5 days per week, Monday through Friday, excluding Wednesday morning. On Wednesday morning the resident will be expected to attend the ED weekly conference. The resident will work under the supervision of attending or senior resident from the Department of Oral Surgery.
Goals and Objectives:
The resident will demonstrate competence in evaluation and treatment of:
1. Oral and dental anatomy
2. Tooth replacement
3. Plastics repair of lip lacerations
4. Odontogenic abscess I&D
5. Local and regional block anesthesia techniques
6. Sialolithiasis
7. Suppurative parotitis
8. Gingivostomatitis
9. Temporomandibular joint disorders
Evaluation:
At the end of the block, the supervising staff will fill out an evaluation form. The resident will also fill out and submit a rotation evaluation form.
Administration Rotation
Faculty Liaison: Dr. Michael Lanigan
Email: Michael.lanigan@downstate.edu
Phone: (201) 916-9494
The administrative block of your senior year is a rotation designed to give you some of the tools and information you will need as you move ahead in your career from resident to attending. The goal of administration is to improve patient care and production while decreasing costs.
1. Structure:
A four-week block (EM) and a two-week block (EM/IM) comprised of tutorials, chart review and meetings. Two weeks prior to the start of your rotation, , please email the following list of people, to inform them of the start of your rotation. CC me on this and any future emails regarding any administrative duties:
Stavile, Brandler, Mehta, and Jackson. Suggested reading lists will be provided upon receipt of your e-mail.
Karen Stavile klstavile@gmail.com
Ninfa Mehta ninfa.mehta@downstate.edu 917-642-6139
Kaedrea Jackson kaedreaj@yahoo.com 917-971-3972
Ethan Brandler ethan.brandler@downstate.edu
2. Chart review:
KCH ED Mortality Review – A Joint Commission requirement is that all institutions analyze “in ED mortality” and complete a brief data sheet regarding the case. Dr. Karen Stavile will be the point person for this activity. She will have a prepared list daily of the mortalities that need to be reviewed and will describe the process for you. This should take approximately 15 minutes to complete (if there are cases to be reviewed).
3. Meetings:
There are many meetings that will be of educational benefit. The following calendar represents required meetings You will be informed about additional administrative meetings that may be pertinent and educational.
Please note during interview season, you will be required to help interview and guide tours for residency applicants on Mondays and Thursdays.
If there is a Rapid Improvement Event (RIE) occurring in KCH during your rotation, you will be required to participate in the full event Monday – Friday 8:30a – 4:30p.
Week Monday Tuesday Wednesday Thursday Friday
1 10:45a
KCH Staff Meeting
S1 Conference Room 8a-12p
Conference
8a-10a
REC
2 10:45a
KCH Staff Meeting
S1 Conference Room
9a-10a
ED to Inpatient (UHB) 8a-12p
Conference
3p-4p
Committee of Patient Complaints (UHB) 8a-10a
REC
3 10:45a
KCH Staff Meeting
S1 Conference Room 8a-12p
Conference
8a-10a
REC
4 10:45a
KCH Staff Meeting
S1 Conference Room 8a-12p
Conference
12:30p-3p
Dr. Rinnert
Graduate Medical Education (GME)
12 noon
Provision of Care
Dr. Lucchesi
2p-4p
Faculty meeting 8a-10a
REC
9a-10a
Performance Improvement
(UHB)
4. Meeting with chairman
Dr. Lucchesi would like to meet with each of the graduating resident during their administrative block. Please schedule this with his secretary at 718-270-2407.
5. Expert Witness:
You may be called upon by hospital counsel to act as an expert witness for a case involving physicians within the Health and Hospitals Corporation. If you are called to do so, please inform Dr. Lanigan and Dr. Rinnert.
6. Residency Performance/Quality Improvement Project:
See below for the ACGME requirements. If you have not completed your project by the time of this rotation please inform Dr. Mehta and/or Dr. Jackson so that they may assist in creating a project to meet the goals of this mandate.
"All residents in ACGME accredited residency programs are required to actively participate in emergency department continuous performance quality improvement programs. Residents must demonstrate evidence of development, implementation, and assessment of a project to improve care. This project may include but is not limited to the development of a clinical pathway, a patient satisfaction survey, or improvement of a recognized problem area. To ensure satisfaction of this requirement, all residents must complete the “Quality Improvement Project Form” which consists of two parts. The first part requires that the resident, under the supervision of a faculty project mentor, complete a proposal for a QI project by May 15th of their PGY3 year for categorical EM residents or PGY4 year for EM/IM residents. The second part requires that the resident complete their QI project by the end of their Administration rotation in their PGY4 year for categorical EM residents or PGY5 year for EM/IM residents. While the requirement may be fulfilled at anytime during the residency prior to the deadlines listed above (i.e. a QI research project or RIE completed during the PGY 2 year), both parts must be signed by the resident, project mentor, and the program director by the stated time frames to satisfy completion of this residency requirement."
7. Absences
Call Dr. Lanigan right away if you anticipate needing to miss any rotation activities during your block. REASONABLE requests made in a timely fashion will be considered though not guaranteed.
EDUCATION
READING
“To see patients without reading is like a ship without a rudder, and to read and not see patients is like never having gone to sea”
-Sir William Osler
“What one knows, one sees.”
-Goethe
Each resident is ultimately responsible for his or her education. Kings County provides a rich environment to practice medicine, but it cannot be stressed enough the importance of reading. Residents must develop a method for acquiring the myriad of information required to competently practice Emergency Medicine. Some people find success with a structured reading list, while others find it more fruitful to do focused reading based on cases seen in the ED. The faculty at Kings County has allowed the residents great autonomy in their clinical education and will not dictate which method of study is best. Also, each of the major Emergency Medicine texts has strengths and weakness. The resident should choose one of the texts and develop a method to comprehensively go through it early in their residency. If you have questions about what to read or methods for review, ask one of the senior residents or faculty members for help.
MODEL OF CLINICAL PRACTICE OF EM
The “old” SAEM core content for EM was felt to be too unwieldy and was thus replaced by “The Model of Clinical Practice of Emergency Medicine”. In essence, it is a similar list as the Core Content but weighted in view of our daily emergency medicine practice as analyzed from over 1300 EM physicians.
It contains three components:
- An assessment of patient acuity
- A description of tasks that must be performed to provide appropriate emergency medical care
- A listing of common conditions
This model was a collaborative effort by the following six organizations governing the practice of EM:
ABEM (American Board of Emergency Medicine)
ACEP (American College of Emergency Medicine)
CORD (Council of Emergency Medicine Residency Directors)
EMRA (Emergency Medicine Resident’s Association)
RRC-EM (Residency Review Committee for Emergency Medicine)
SAEM (Society of Academic Emergency Medicine)
The actual document is too long to be printed here but may be easily accessioned at:
http://saem.org/download/practice.pdf
Reading this document gives you a good insight about what you should learn over the next four years or what you should know when graduating from your residency
IN-SERVICE EXAMINATION
The national emergency medicine in-service exam is held every year on the last Wednesday of February. The exam format is similar to the ABEM written examination. The exam is a 4.5 hour-long multiple-choice exam containing approximately 210 questions. While the exam is not perfect and does not necessarily predict who will become a competent clinician, the exam is written by the same question writers who contribute to the specialty board exam. Therefore, performance on the In-service Exam correlates exceptionally well with success on the ABEM written exam (see attached graph).
Proper preparation requires an ongoing effort of reading on core topics in Emergency Medicine and reviewing board-type questions. A strong fund of knowledge will be required to perform well on the in-service exam and the best preparation is to start early in your residency with regular reading and review. Residents who do not perform well on the examination when compared to the national average for their respective PGY year, are not eligible for exemption from the In-training and Board prep conference. Please see the section on that conference elsewhere in this book.
Please Note: No vacation or away electives can be scheduled during In-service exam week. You MUST take this exam.
Recommended Reading:
Tintinalli – Emergency Medicine study guide
Rivers, Carol – Preparing for the Written Board Exam, text and questions
Peer VII questions
Koenig – Emergency Medicine Pretest Self-Assessment and Review
Pearls of Wisdom – Emergency Medicine Written Board Review
Rosen-- Text of EM

BOARD REVIEW GROUP
EM Faculty Liaisons:
Dr. Joel Gernsheimer (cell: 917-750-1145, pager: 917-219-1976,
email: gernsh@aol.com)
Dr. Antonia Quinn (email: antonia424@earthlink.net)
Dr. Binita Shah (email: binita1@hotmail.com) - pediatric liaison
Description and Goals: Participation in Board Review Group is an opportunity for residents to enhance their preparation for the yearly in-service examination and for the ABEM written board examination. The goals of this activity are to:
• Improve medical knowledge
• Improve test taking skills
• Improve scores on the annual In-Service Exams
• Improve scores on the ABEM Board Certification Examinations
All residents must attend. You may opt out of attending this group if you meet any one of the following criteria:
You score above a 79% on the In-service exam.
You score above the National Mean for your PGY level.
You are an EM/IM PGY1 and score above the 14th percentile of PGY1s nationally.
You are an EM/IM PGY2 and score above the 14th percentile of PGY2s nationally.
You are an EM/IM PGY3 and score above the 29th percentile of PGY3s nationally.
Please note that all Interns are automatically included in this group.
Please note that PGY4 EM Residents and PGY5 EM/IM Residents who scored below the national mean for their PGY level are no longer allowed to opt out of this group to do their own study plan.
Please note that if there is a question regarding the eligibility of a Resident to opt out of the Board Review Group, the final decision for EM Residents will be made by the EM Categorical Program Director, and for EM / IM Residents by the EM / IM Program Director.
Sessions are held at least twice monthly, and the discussed topics are prepared by assigned residents. The format is a review of board-style questions, test taking strategies and topic content.
Meeting place/time: The Board Review Group meets every other week (usually the first, third and fifth Wednesdays of the month) from July through June for one hour immediately after Wednesday conference (12:15 to 1:15). This may sometimes be changed, because of holidays or “away conferences”. You may bring your lunch. A detailed schedule will be handed out at the first meeting and may be revised throughout the year. If you are scheduled for a clinical shift immediately after conference, you must let the attending in the clinical area know prior to the beginning of your shift that you will be one hour “late”. Sometimes the clinical attending will insist that you go to the clinical area immediately, if he or she feels that attending the session will affect patient care adversely. Any conflict should be discussed with Dr. Quinn or Dr. Gernsheimer.
If you cannot attend Board Review Group for whatever reason you must notify Dr. Quinn or Dr. Gernsheimer by email or phone or in person.
The reasons to be excused from a particular Board Review Group Session are the same ones as for being excused from the morning Conferences (annual leave, being ill, working in the ICU, etc.), but you still must notify Dr. Quinn or Dr. Gernsheimer and let them know this, before Mid-night of the day of that particular Board Review Group session, or you will owe 4 hours. For every 2 sessions you miss without notifying Dr. Quinn or Dr. Gernsheimer, you will be given an 8 hour clinical shift.
Please note that if you are assigned to do a Simulation Session that day, you should come to the Board Review Group at 12:15 and then go to the Simulation Session at 12:30.
Attendance is mandatory for all residents in both programs (unless you are eligible to opt out) and will be taken.
Sessions are usually held in either the CTC conference room or our main EM conference room. You will be notified prior to each session where that session will be held.
Structure:
Residents will be assigned their topics for review in July. Attempts to follow the Modular Curriculum Schedule, as much as possible, will be made.
The assigned residents for each session will prepare 5 -10 multiple-choice questions each (using Peer VII or V111, Rivers, Tintinalli, Just the Facts, 1000 (now also 1200) Questions to Help You Pass the Emergency Medicine Boards, Emergency Medicine Pearls of Wisdom, Last Minute Emergency Medicine or other sources), so that there are at least 15 - 20 questions for each session. Each assigned resident will email his or her questions and answers to the Team Leader at least 9 days (or sooner if the Team Leader feels he or she needs more time) prior to that particular session, so that the Team Leader for that session has the time to put all the questions together, including his or her own, and email them out to all the residents (either via the drop box or SUNYEM) at least 7 days prior to that session. The Team Leader for each session will be marked on the Board Review Schedule, and will be the first name listed on each session’s schedule. In addition to making his or her own questions, the Team Leader is expected to put together all the questions, he or she receives from the other Team Members together in one document, making sure that there are no duplicate questions and that the questions are appropriate, and send them out to all the residents, Dr. Quinn and Dr. Gernsheimer, no later than 12 Midnight of the Wednesday, one week prior to that session. The Team Leader, as noted below, will also send out the answers in one document to Dr. Quinn and Dr. Gernsheimer (and Dr. Shah for the Pediatric, Dermatology and Stimulus sessions) at least one week prior to that session. This will allow for adequate time to review and answer the questions for that topic. Everyone is expected to read up on the topic prior to Board Review Group, but the residents who prepare the topics are expected to be experts on these topics and lead the discussions and expand on the answers. Just preparing questions is not enough. Remember, the more you put in, the more you will get out of this educational experience. Residents preparing the topics will be matched with topics that they appear to be weaker in, as per their results on the In-Service exam. A resident may be assigned to do questions and be the expert on more than one topic.
Also please note that starting this academic year, all the residents who are in the Board Review Group will answer the questions and send the answers to Dr. Quinn and Dr. Gernsheimer, no later than Midnight of the Monday right before that week’s session. This will include even the residents who are excused from attending the session, because they are working nights or are off service. This is being done, because we noticed that many residents are not getting the benefit of these sessions, because they are excused. We have also noticed that many residents are coming to the sessions unprepared, and not having even read the questions. Residents, who do not send the answers in to us by the Monday night deadline, will be given the 4 hour penalty as explained above for other failures to meet deadlines.
The only exception to this will be residents on annual leave, or who are out of the country on a special international elective. Even then you must notify us of these facts, or you will get a penalty. Dr. Quinn will set up a special drop box to make it easier for residents to submit their answers.
Answers to the questions with explanations should be provided to everyone After the end of the session on the day of Board Review Group by the Team Leader via email or drop box, so that “when we go around the room” asking questions to the other residents in the group, they need to have read on the topic, and not just read the answers. The assigned resident will discuss the answers to the questions he/she prepared in more detail, and add expertise to the topic. The attending present will provide additional insight into the subject matter and attempt to resolve any "conflicts" regarding answers. This will require active participation by everyone and create an environment conducive to learning.
Please note that Dr. Michael Ritchie has kindly agreed to post the questions and answers on Clinical Monster after each session.
As noted above, Questions and Answers must be given to Drs. Quinn and Gernsheimer at least one week prior to that Board Review Group session by the Team Leader, who will insure that the questions are appropriate and duplication of questions are prevented. If the Team Leader or any of the Team require assistance in making the questions, or have any questions regarding the appropriateness of the questions, then they should contact either Dr. Gernsheimer or Dr. Quinn for help prior to sending out the questions. Again note that starting this academic year all the residents should “take the test and submit answers” to Dr. Quinn and Dr. Gernsheimer at least 2 days prior to that week’s session.
Please note that 3-5 questions on that topic should be related to Pediatric Emergencies.
Large topics such as Trauma, Cardiology, Respiratory and GI will have more than one session devoted to them.
It should also be noted that residents who are assigned to do questions and answers for a session must get them in, and distributed within the required times as noted above. Any assigned resident who misses the required deadlines will owe 4 hours for each session that they did NOT make the deadline for. Two sessions of unexcused absences or missing deadlines or any combination of these will lead to having to do an 8 hour clinical shift.
Please note that even if you are excused from attending a session for any reason, but were assigned to make questions and answers, then you must do your questions and answers and submit them on time, even if you are not physically attending that session.
The first meeting of the Board Review Group in August will be devoted to going over the goals and the rules of the group, and will also be a “Study & Test Taking Skills Session”. The residents (not the interns, although they will be expected to attend this session) included in this group will be expected to bring a “study plan”, which addresses their academic weaknesses, as indicated by the areas in the In-Service Exam that they did poorly in. Faculty will be available to assist the residents with formulating and carrying out their study plans. The second session will be devoted to reviewing a “ Mock Board Review Test” that will be distributed by Dr. Gernsheimer one week prior to the second session. Residents in the group will be expected to take this “Mock Test” and submit the answers to Dr. Quinn and Dr. Gernsheimer at least 2 days prior to the second session.
Finally, it should be noted that each session of this group will count as an hour of Self Directed Learning. Even residents, who have the choice to opt out of the group, can still attend it in order to earn Self Directed Learning hours (although they will not be assigned questions & answers to do and submit). Attendance will be taken to verify that the residents actually attended these sessions, and deserve credit for this activity. Residents who attend the sessions should send the requests for asynchronous learning credits to Dr. Gernsheimer via New Innovations. We wholeheartedly encourage all residents to attend these sessions, and gain these asynchronous learning hours.
Any questions or suggestions should be brought up to Dr. Quinn and/or Dr. Gernsheimer, as we greatly value your input.
Again, we would like to emphasize that it is very important to get the questions and answers in on time, and to inform us when you cannot attend a session. Because we cannot check the schedule for every resident in the group, it is important that you let us know when you cannot attend, even when you have a valid excuse. We do not want to give out “penalty shifts”, so please follow all the rules noted above, so we do not have to do so. Your cooperation and compliance with all the above is greatly appreciated. Thank you.
Copies of PEER V111, 1000 and 1200 Questions to Pass the EM Boards, Last Minute Emergency Medicine, Just the Facts, and EM Pearls of Wisdom will be made available for your use via Dr. Gernsheimer. Please contact him if you would like to review any of these very useful review books.
EMERGENCY MEDICINE BOARD EXAMINATION
The American Board of Emergency Medicine certification exam is the final exam hurdle to full board certification in EM. The exam is a two-part exam taken upon completion of an accredited residency training program in EM. The first part of the exam is a written test given in the fall (typically the first week in November) at a national computer testing center. The written exam is a six and a half (6.5) hour, 340 criteria referenced question exam. The candidate must answer 80% of the questions correctly to pass the exam. The scope and depth of the exam is similar to that of the annual in-service exam.
The oral certification exam is offered to candidates who successfully complete the written exam. The exam is offered in the spring (late April) and the fall (early October). Assignment to the spring or fall exams is completely random. The exam is a three and a half (3.5) hour test consisting of seven patient encounters (single or multiple patients) lasting 15 to 40 minutes in duration.
Residents will receive an information packet from ABEM in the spring of their final year that contains an application and fee schedule. The written exam is about $1,300 (this includes a $290 application fee), and the oral exam is approximately $1160.
The big question is how and what to study. The good news is that most people who graduate from an EM residency will pass the exam (last year’s pass rate was 95%). One may be able to roughly predict their degree of preparedness based on the yearly in-service exam. To restate from the previous sections of this handbook, the best method of obtaining the required information to pass the exams is to develop good reading habits early in residency.
Most people spend a considerable amount of time in the fall after graduation preparing for the exam but the four years of residency is the time to obtain the core knowledge required to be a competent EM physician. Details about the exam are probably best referred to the residency directors or recent graduates who are taking the exam.
Contact:
American Board of Emergency Medicine (ABEM)
3000 Coolidge Road
East Lansing, Michigan 48823-6319
Tel: 517-332-4800
Fax: 517-332-2234
www.abem.org
ABEM WRITTEN EXAM CONTENT
Signs, Symptoms and Presentations |
9% |
Cardiovascular disorders |
10% |
Cutaneous disorders |
2% |
Endocrine/metabolic/ nutrition disorders |
3% |
Environmental disorders |
3% |
ENT disorders |
5% |
Hematologic disorders |
2% |
Immune disorders |
2% |
Systemic infectious disorders |
5% |
Musculoskeletal disorders (not trauma) |
3% |
Nervous system disorders |
5% |
Obstetrics and Gynecology |
4% |
Pediatrics disorders |
8% |
Psychobehavioral disorders |
3% |
Renal and Urogenital disorders |
3% |
Thoracic/respiratory disorders |
8% |
Toxicology |
4% |
Trauma disorders |
11% |
Administrative |
2% |
EMS/disaster |
3% |
Clinical Pharmacology |
2% |
Procedure/Skills
|
6%
|
USMLE EXAMINATION REQUIREMENTS
Residents must have passed USMLE step I & II before matriculation in residency and most will take and pass part III during the early years of residency. Applications may be acquired from NY State Board of Education by calling (518) 474-3817.
Passing Step III will be required by the end of your 2nd year of residency and is part of your promotion criteria into the PGY3 year in the categorical and the combined programs.
Passing Step III is required for obtaining a medical license in every state.
SUNY has set up an institution-wide policy. If for some reason you have not PASSED Step 3 by the end of your PGY-3 year, then SUNY GME will terminate your contract. This means you are no longer a part of the residency. I am not kidding.
If you have not passed Step-3 by the beginning of your PGY-3 year, you will be given a notice of non-renewal in November of your PGY-3 year, which I can have rescinded if you pass Step 3 before the end of the academic year.
You do not have to apply for a New York state medical license in order to be promoted, but you are strongly encouraged to. A NYS medical license is required to be a chief resident and is required to moonlight outside of our system.
New York (NY) State no longer requires licensing fees and NY state application at the time of registration for the exam (about $600), i.e. you may sit for Step III without applying for NY state licensure. CIR will reimburse your costs of getting a license.
DEPARTMENT CONFERENCES
MORNING REPORT
Morning report gives the opportunity to discuss interesting cases that present to the ED in a relatively formalized manner. It is an excellent educational forum for the residents and faculty and a time for a brief discussion of both core topics in emergency medicine as well as evolving medical therapies.
Faculty Liaison: Dr. Jay Khadpe
Time and Place:
Morning report is to be held following morning rounds on Mondays, Tuesdays, Thursdays, and Fridays in a location designated by the attending physicians (usually adult or pediatric trauma bay in CCT).
Structure:
• Only senior residents will be asked to present a case for discussion. Any one resident should be required to do no more than two morning reports during a single ED block. The resident scheduled to present will be designated on the schedule.
• The Pediatric ER attending will present the morning report on Thursdays.
• All residents scheduled to work at 7 AM or who are post-overnight at KCH ED are required to attend. Residents scheduled at UHB at 7 AM are encouraged to attend at the discretion of the UHB Attending. Residents must first report to UHB for rounds and are to report back promptly at the conclusion of the case.
• The fourth-year administrative resident is required to attend half of all morning reports, to take attendance and to note the topic and presenter. This information must be given to Dr. Lanigan each week.
• The resident presenting the morning report is required to submit a brief write-up to Dr. Khadpe on each topic that he/she presents. The write-up should consist of a brief summary of the case with the pertinent teaching points highlighted. This write-up will be posted on Clinical Monster for the benefit of the residency.
The purpose of the exercise is to provide the presenter an opportunity to present a case that he/she was personally involved with and to educate his/her colleagues. The objective of the presenter is to extract the most essential Emergency Medicine teaching points and convey these to the group. In order to accomplish this goal, we have decided to initiate some guidelines to follow in preparing your morning report:
1) Morning report should NOT be presented in an Oral Board format. The total presentation time should not exceed 10-15 minutes depending on patient needs. Remember there are residents and faculty present who worked overnight and do not want to hear a long presentation.
2) The first 5 minutes should be devoted to a case presentation by the presenter. This is not a history-taking lesson nor is it a free-for-all guessing game. The presenter will provide all pertinent positive and negative historical facts at his/her discretion. He/she can stop at any time to elicit specific interventions at any time—life-saving procedures, etc.—but the primary focus of this portion is to provide all the necessary information for the second part of the case.
3) The group should then be pressed to provide a differential diagnosis—either round robin or by picking specific audience members, preferably the most junior first (MS3, MS4, PGYI, etc.). Obviously, focus on any life- or limb-threatening injuries, diagnoses, or interventions first, and be as complete as possible.
4) Finally, the presenter will spend no more than 5 minutes highlighting the most important points that each person in the room should walk away with (at least three). This should be concise and to-the-point, and SHOULD BE ACCOMPANIED BY SOME TYPE OF HANDOUT OR STIMULUS (copies of EKG’s, X-RAY’s, diagrams etc.).
5) If morning report has not finished by 8am, the individuals that worked the previous overnight shift that are in attendance are excused and may leave to head home regardless of when the morning report started.
WEDNESDAY CONFERENCE
The Wednesday conference is the traditional EM academic conference that attempts to cover the core topics in emergency medicine over approximately a two-year period. Conference for EM residents will be held each Wednesday from 8am – 12pm. The schedule will be published every 6 weeks (by module) by Education Chief. The conference is composed of various didactic lectures covering the core curriculum of emergency medicine, specialized case discussions pertaining to pediatrics, the MICU and trauma, journal club, a morbidity and mortality conference, an annual CPC competition, and grand rounds. The curriculum will be covered in a modular format keeping a consistent topic for each 6-week period.
ALL RESIDENT LECTURES MUST BE E-MAILED TO THE CONFERENCE LEADERS FOR REVIEW ONE WEEK BEFORE TO CONFERENCE (Clinical Pearls requires topics to be sent two weeks prior, and you will be advised about the preparation requirements for CBL literature review well in advance and must comply). PLEASE CC EDUCATIONAL CHIEF Cassandra Bradby (cassandra.bradby@gmail.com) WHEN SUBMITTING YOUR LECTURES.
Conference attendance is mandatory.
RRC requires that every EM resident must be present for 70% of the Wednesday conferences during your residency training (35% for EM/IM residents). The attendance statistics will be posted on the conference room door approximately every quarter. Persons who are repeatedly late will be marked as absent (3 tardiness marks = one extra clinical shift). Please refer to the latest Conference Attendance Policy and ACGME/NY State guidelines based on clinical shifts below.
Special Shifts and Wednesday Conference
Junior residents (PGY 1 and PGY 2) will have the majority of Tuesday PM shifts off to enable their attendance at conference. Residents have to report to the clinical area immediately after conference. Senior residents may be scheduled for one Tuesday overnight, one Wednesday AM and/or Wednesday PM shifts as coverage dictates. The scheduling chief resident may have the residents scheduled for shortened shifts after conference as coverage dictates. Senior shifts scheduled 11AM – 7PM and Junior shifts scheduled 7AM-7PM begin at 12 Noon.
The following are the updated requirements for conference attendance that take into account resident work hours and current ACGME and NY State guidelines. If you have any questions as to whether or not you need to attend conference please contact Dr. Teresa Smith (teresaemergencymd@gmail.com)
ACGME and NY State guidelines
KCH
Tuesday Shift Wednesday Shift Attend Conference
Off 3PM-11PM 8AM-Noon
Off 11PM-7AM 8AM-11AM
Off 7PM-7AM Off
7AM-3PM 3PM-11PM 8AM-Noon
7AM-3PM 11PM-7AM 8AM-Noon
7AM-7PM 7AM-7PM 8AM-Noon
7AM-7PM 7PM-7AM Off
9AM-9PM Off 8AM-Noon
11AM-11PM Off 9:30AM-Noon
11AM-11PM 11AM-11PM 9:30AM-Noon
11AM-11PM 7PM-7AM Off
3PM-11PM Off 9:30 AM-Noon
3PM-11PM 3PM-11PM 9:30 AM-Noon
3PM-11PM 11PM-7AM 9:30 AM-Noon
7PM-7AM Off 8AM-9AM
7PM-7AM 7PM-7AM Off
11PM-7AM 11PM-7AM 8AM-9AM
11PM-7AM Off 8AM-9AM
UHB
Tuesday Shift Wednesday Shift Attend Conference
7AM-5PM Off 8AM-Noon
7AM-5PM 12PM-7PM 8AM-Noon
7AM-5PM 3PM-11PM 8AM-Noon
7AM-5PM 11PM-7AM 8AM-Noon
11AM-9PM Off 8AM-Noon
11AM-9PM 12PM-7PM 8AM-Noon
11AM-9PM 3PM-11PM 8AM-Noon
11AM-9PM 11PM-7AM 8AM-Noon
1PM-11PM Off 9:30AM-Noon
1PM-11PM 12PM-7PM 9:30AM-Noon
1PM-11PM 11PM-7AM 9:30AM-Noon
11PM-7AM Off 8AM-9AM
11PM-7AM 11PM-7AM 8AM-9AM
Every effort will be made to allow residents maximum conference attendance without compromising patient care.
Off-service Rotations:
For non-KCH sites and off-service rotations, please refer to the Clinical Responsibilities section of this handbook under the specific rotation heading for specific schedule information. In general, on the non-ED off-service rotations during the first two years residents will act as full members of the off-service clinical staff and have similar clinic and call schedules. For all off-service rotations at KCHC, excluding the ICU rotations, the resident is expected to attend conference for at least 2 hours – this is a required part of education and should be excused by the off-service team.
ED CONFERENCE ATTENDANCE POLICY
Conference attendance is mandatory. RRC requires that every EM resident must be present for 70% of the Wednesday conferences during your residency training (35% for EM/IM residents). Please refer to Conference Attendance Policy for attendance requirements.
You can meet the 70% requirement through a combination of asynchronous (independent) activities and traditional didactic lectures. You must have 182 hours of total conference (asynchronous and traditional) time per year. This must include at least 132 hours of traditional conference time (you can do more). 132 hours is equal to 33 weeks of conference time. You will get 4 hours of credit each week you show up based on the rules in the previous section of the handbook. Additionally, you can get credit for up to 52 hours via asynchronous learning. See below for rules regarding asynchronous learning.
INDEPENDENT STUDY
Individualized Interactive Instruction (Asynchronous Learning) Program: Each resident must complete a minimum of 36 hours prior to May 15th of each respective academic year for the purposes of promotion and/or graduation [maximum of 52 hours per academic year counted from July 1st to June 30th (70% of those hours are required toward satisfaction of the overall conference requirement)]:
Online Conference Modules: Each online module will contain multiple activities posted on clinicalmonster.com/moodle. Each resident will receive 1 hour of credit for completion of each activity within a module. To receive credit for each activity, the resident must read the corresponding posted articles, participate in the online discussion of the articles on nb.mit.edu (free registration), pass the online quiz (a minimum score of 70% is considered passing), and log their completion in New Innovations* selecting Dr. Khadpe as the supervisor. There will also be a pediatrics module for each academic year that covers topics for all the Wednesday conference modules during that year.
EB Medicine: Each resident has free access via their EMRA membership to ebmedicine.net. Each resident will receive 1 hour of credit for each completed article. To receive credit, you must submit the CME certificate along with a list of 3 clinical pearls you learned to your designated Dropbox folder (see clinicalmonster.com for a detailed description of how to setup your Dropbox folder) and log your submission in New Innovations* selecting Dr. Khadpe as the supervisor. Each resident may receive credit up to a maximum of 20 hours per academic year for this activity.
Board Review: Each resident will receive 1 hour of credit for each session. You must log your attendance in New Innovations* and select the supervising attending to verify your attendance and receive credit.
Simulation: Each resident will receive 1 hour of credit for each simulation session. This also includes Trauma Simulation, Procedure Simulation, and Cadaver Lab sessions. You must log your attendance in New Innovations* and select the supervising attending to verify your attendance and receive credit.
Pediatric EM Fellowship Conference: Each resident will receive 1 hour of credit for each hour of attendance at the PEM conference (maximum of 3 hours per week). You must log your attendance for each hour of participation in New Innovations* and select the supervising attending to verify your attendance and receive credit.
Food and Journal Club: Each resident will receive 1 hour of credit for each meeting. You must log your attendance in New Innovations* and select the supervising attending (usually Dr. Wiener) to verify your attendance and receive credit.
NYCPCC Consultants Conference: Each resident will receive 2 hours of credit for each conference attended. You must RSVP to Dr. Wiener in advance to ensure that he will be present to verify your attendance. You will not receive credit for attending this conference during your toxicology rotation, as this is already a requirement for that rotation. You must log your attendance in New Innovations* and select Dr. Wiener to verify your attendance and receive credit.
Slit Lamp Sessions: Each resident will receive 1 hour of credit for each session. You must log your attendance in New Innovations* and select the supervising attending (usually Dr. Silverberg) to verify your attendance and receive credit.
Mini-Fellowship Conferences: Each resident will receive 1 hour of credit for each meeting. You must log your attendance in New Innovations* and select the supervising attending to verify your attendance and receive credit.
IMSAL Advanced Airway Skills Course: Each resident will receive 4 hours of credit for completing the course. To receive credit, you must submit the CME certificate to your designated Dropbox folder and log your participation in New Innovations* selecting Dr. Papanagnou as the supervisor.
Note: Credit may be given for select outside conferences on a case by case basis if it complies with RRC requirements. In order to receive credit in these instances, approval must be given by the Program Director or his/her designee prior to participation at the conference.
*How to log asynchronous credit in New Innovations: For each 1 hour of credit, you must input a separate entry in the "Procedure Logger" selecting "1 Hour Asynchronous Learning" as the procedure. The following is a list of required fields to complete for each entry:
1. Patient ID: NA
2. Last Name: NA
3. Patient Type: Asynchronous Learning
4. Date Performed: Date activity was completed
5. Procedure: 1 Hour Asynchronous Learning
6. Supervisor: Name of supervising attending
7. Role: Performed Procedure
8. Diagnosis Text: Name of activity completed - be specific! (i.e. Title of EB Medicine article completed or name of specific module quiz completed)
If the activity is worth more than 1 hour of credit, you must log the activity an additional time for each additional hour of credit (i.e. upon completion of the IMSAL Advanced Airway Skills Course, you would log the activity 4 times to receive all 4 hours of credit). You will receive credit upon verification by the supervising attending of your participation and satisfactory completion of the activity.
Notice: If an entry in New Innovations is incomplete or incorrectly submitted, it will be deleted upon review.
PRESENTATION PREPERATION POLICY
Resident lecture presentation is an integral part of resident education. Resident presentation allows resident to become experts in the topic discussed. In addition, learning how to give a presentation becomes the foundation of your educational experience. For those continuing careers in academics, giving lectures will be large amount of your non-clinical responsibilities, thus this becomes important part of our residency education. Resident presentations should be viewed as a professional event, where proper business casual attire and behavior is required.
Lectures must be submitted to Senior Lecture Coordinators, Faculty Lecture Advisor, and Educational Chief (Cassandra Bradby cassandra.bradby@gmail.com). A period of 1 week should provide ample time for feedback and adjustment (see above for submission requirements).
We realize that you may have other obligations the month before or the month of your presentation. Therefore, you will need to plan ahead to make sure you have adequate time to prepare your presentation and have it submitted for review 1 week (7 days) prior to your presentation. The yearly schedule of presentations is published on the residency bulletin board and can also usually be found below the Educations chief’s "signature" on their emails. Please contact Dr. Smith (teresaemergencymd@gmail.com) well in advance if there any issues with presentation preparation; particularly, if there is no response with feedback from Senior Resident Lecture Coordinator or Faculty Advisor.
Below is the description/update to Resident Lecture Conference Series 2013-2014 academic year:
Resident Lecture Series
Clinical Pearls: will be two 30-minute talks during one conference day. The talks will be given by a first year resident only, with the option of covering one of three topics: Fast Track Pearls, Procedural Pearls, and “Bread and Butter” Emergency Medicine. No power point presentations will be allowed. Each presenter will give a case presentation from a case they saw clinically. The case must cover one of the three main themes above. A scriber will dictate pertinent information on the white board during the presentation. In an interactive case presentation format, the audience will be guided to ask for more clinical information in order to formulate a differential diagnosis. After the audience formulates a differential diagnosis, the presenter will give the final imaging, ECG, and labs that helped synch the diagnosis. The presenter will spend 5 minutes summarizing the case and giving the clinical pearls of the disease entity using handouts or visuals as needed. Senior Coordinators: Hannah LoCascio, Kevin Ting, Sadia Hussain Advisor: Teresa Smith
Adult Journal Club: In order to increase audience participation, the key objective is to provide the article and the discussion in variety of formats. The journal club discussion will start the two weeks prior to conference on The Original Kings of County Blog. By increasing advertisement for the blog, we hope to increase traffic to the blog site, and have more Faculty participation. In addition, the article will be sent via email to the faculty and resident list serve two weeks prior to conference. We will encourage residents to also provide the podcast if available for the article as well. During conference, we will display the blog and responses posted during the article presentation. In addition, the resident presenting the journal club article will choose one statistical component to go over with that article, i.e., is this article powered enough to provide the evidence for the research question? The presenter will then discuss the definition of power. Senior Coordinators: Adam Aluisio, Joseph Freedman, Richard Shin Advisor: Teresa Smith, Antonia Quinn
Topic Review: Will be based on published board review questions from various sources including PEER XIII, 1000 EM Questions, etc. We will be purchasing several question books for this purpose and board review (email Cassandra Bradby or Teresa Smith in advance to borrow). The Senior resident will have the option of presenting these questions in a Jeopardy format. Or, the resident may choose a small group format where the questions are divided and answered amongst a small group, after which the answers are discussed as the larger audience. Topic Review will require the use of audience response technology (“clicker”). For instructions and preparation please contact Cassandra Bradby. Answers to all questions must have a thorough explanation. Both questions and answers must be made available after conference in power point format to be uploaded to Clinical Monster for future review by residents. Senior Coordinators: Cassandra Bradby Advisor: Joel Gernsheimer
Simulation
Current Format: The current format for the SIM "lecture" series as part of weekly conference is a monthly session in which four residents are chosen to participate in a 15-20 minute SIM session in the simulation lab. The case is chosen based on the system, or "module" on which the didactics are focused for that month. For example, during the pediatrics conference the case was one of an extramural delivery of an infant who was in respiratory distress. The residents work through the case in the simulation lab with a faculty member who runs the case from the sim control room. The faculty member controls the simulation models actions, provides data such as vital signs and laboratory and imaging results, and plays the part of anyone with whom the team leader speaks with over the phone, for example consultants or EMS providers. There is also a sim assistant who plays the role of a nurse or consultant in the room. This person provides equipment for necessary procedures and helps to guide the resuscitation while allowing the team leader to run the case. The remainder of the conference attendees watches as the case progresses over CCTV in the conference room. Once the case reaches its conclusion, the residents return to the conference room for a short debriefing session in which their performance is analyzed. This is followed by a 30min lecture about the subject matter of the case. Senior Coordinators: Linda Fan, Clare Desmond, Randi Ozaki, Julie Waldman Advisor: Sigrid Wolfram, Jessica Stetz
Recommended Changes: 1. Occasionally more than one case at time to simulate multi-tasking environment of ED. 2. Identify and assign senior group leader prior to conference. Every 4th year can be pre-assigned and notified prior to conference that they will be actively participating the simulation conference that day. 3. The didactic lecture should better reference the events of the sim case itself. The weekly sim session debriefings typically are accompanied by a critical action checklist and the management of the case is critiqued through this lens. The lecture, if given in this format, could help summarize and organize the appropriate management of the patient in question. 4. The debriefing session should also follow the critical actions checklist format.
ICU Conference:
Current Format: 45min to 1hour, two resident presentations: Junior resident presents the case for 15 minutes. Senior resident presents a pertinent topic for 35-40 mins.
Recommended Changes: Now one resident presentation. Senior resident presents the case with learning points. 15 – 20 minute faculty commentary (DeSouza) at the end of the presentation. This will allow one senior presenter to bring the case together with learning points rather than making the presentation segmental. It will limit interjections and make the presentation run smoothly. The faculty commentary will be a short time period for an attending to present advanced learning points, commentary from audience and facilitate discussion. Senior Coordinators: Francis Youn, Eugene Kang, Andy Grock Advisor: Ian DeSouza
M&M
Current Format: Two Senior level presenters review a case each for 30 minutes each. Usually there is commentary during the presentation. The final words are usually about error and the types of error performed in the case are discussed. Small amount of learning points are reviewed if time.
Recommended changes: Presentation should have focus on the medicine involved in the presentation, the thinking involved in the medical error and differences that could have prevented the error. Faculty should be asked to hold all commentary to the end of the presentation, so as to allow the learning points to be discussed without interruption of the case. Senior Coordinators: Baruch Berzon Carl Alsup, Marsha Lewis Advisor: Joshua Schechter
Core Content
Current Format: Lecture given by EM/IM based on basic emergency medicine concepts. Often turns into evidence based medicine lectures, where there is a clinical question and the presenter uses current literature to answer this question.
Recommended Format: Lecture should be given by an EM/IM or Second year EM resident. This should be lecture based on current practice guidelines of frequently seen emergency medicine cases. This lecture should discuss a basic of the emergency medicine topic, and merge what the current literature states should be our daily medicals practice. Senior Coordinators: Michael Ritchie, Adam Nordstrom, Eli Brown Advisor: Claritza Rios
CBL:
Current Format: Residents are presented with a case vignette two weeks prior to conference. Selected residents are asked one month prior to find journal articles that answer clinical questions based on the vignette. Each question is written for PGY year level, with the first year question being more basic review of the topic and the more advanced years addressing questions with more specific currently debated topics. The case vignette and journal articles are provide to the residency one week prior. Residents are expected to be familiar with their year’s clinical question and journal articles, and to present these in a small group format on the day of conference. Faculty led the small groups, which are randomly assigned the morning of conference.
Recommended Format: 1. There should be a limit of two journal articles each question. 2. Residents should be pre-assigned to small groups and these assignments should change once throughout the year. 3. Faculty small group leaders should receive a summary of the articles one week prior to the conference. Senior Coordinators: Ambert Louis, Nathan Reisman, Pia Daniel Advisor: Jennifer Martindale
Senior Lecture: Given by a fourth year resident to discuss whichever topic they choose. Most highlight their learning lessons from residency or topics in which they have interest, and have developed through their four years. Senior Coordinators: Cassandra Bradby Advisor: Jay Khadpe
SENIOR RESIDENT LECTURES
All 3rd and 4th year residents will give several lectures throughout the academic year.
Senior residents will be assigned to act as Senior Resident Coordinators for resident lecture series. As part of their Senior level educational responsibilities, senior residents must review and advise juniors on their presentations. Seniors must work in conjunction with the Lecture Faculty Advisor on how presentations will be reviewed and what their expectations are as the Senior Coordinator for their assigned conference series. Active participation is required.
See Wednesday Conference section titled: Presentation Preparation Policy. Synopsis is that conference presentations are to be taken as professional events, which prepare you to teach in an academic setting, and present nationally.
4th year: Senior Lecture: Given by a fourth year resident to discuss whichever topic they choose. Most highlight their learning lessons from residency or topics in which they have interest, and have developed through their four years. Senior Coordinators: Cassandra Bradby Faculty Advisor: Jay Khadpe
The schedule for Senior Resident Lectures and resident presenters will be posted and distributed by the education chief resident.
MISCELLANEOUS POLICIES AND PROCEDURES
RESIDENT RESPONSIBILITIES AND DUTIES
In accordance with the recommendations of the Accreditation Council for Graduate Medical Education (ACGME), and the SUNY-Downstate Graduate Medical Education Committee, the resident will be provided with an opportunity to:
1) Develop a personal program of self-study and professional growth with guidance from the teaching staff.
2) Participate in safe, effective, and compassionate patient care, under supervision, commensurate with their level of advancement and responsibility.
3) Participate fully in the educational scholarly activities of their program and, as required, assume responsibility for teaching and supervision of other residents and students.
4) Participate in institutional programs and activities involving the medical staff and adhere to established practices, procedures, and policies of the institution.
5) Participate in institutional committees and councils, especially those that relate to patient care review activities.
6) Participate in evaluation of the quality of education provided by the program.
7) Develop an understanding of ethical, socioeconomic, and medical/legal issues that affect graduate medical education and of how to apply cost containment measures in the provision of patient care.
8) Residents shall perform their duties and at all times conduct themselves in compliance with all applicable departmental rules and regulations, as well as applicable Hospital policies and procedures, both personnel and operational, and such specific rules and regulations.
It is therefore expected that the resident always act in a professional manner. Dishonesty, disinterest, and unkindness are serious offenses and may be grounds for dismissal from the program.
Policy on Eligibility and Selection of Residents
Candidates for residency will have graduated an LCME-accredited medical school or a medical school fulfilling ECFMG standards. Candidates will have passed the USMLE step 2 or the Complex Step 2 prior to entry into the training program. Residents will hold a medical degree from an allopathic or osteopathic medical school or an equivalent degree if from a foreign medical school.
All applications for PGY1 positions are accepted through the ERAS program. At the discretion of the Program Director, residents may also enter the program through special international education programs. These residents may function outside or as part of the main residency program. The Residency Director and the Assistant Directors screen completed applications for specific criteria. Interviews are offered to approximately 200 applicants based on their personal statement, letters of recommendation, board scores, transcripts and dean’s letter. Interviews are held twice a week, with 10 applicants per session. Applicants are given an introductory slide presentation, which describes the key aspects of the program including the length of the program. Usually, the residency director, and the assistant residency directors, and a resident interview candidates. The interviews are one on one or two on one and run approximately 20 minutes each. During the interview day, applicants are offered an opportunity to meet with residents for a question/answer session and tour of the facilities. Recruitment for the combined program is done similarly in concert with the Internal Medicine Program Director.
The Interviewers rank the applicants based on their prior academic performance and future growth potential, their interview presence and interpersonal skills, their commitment to Emergency Medicine, ethnic and cultural diversity, and the desire to work and learn in an inner city hospital environment.
PROMOTION/GRADUATION CRITERIA
Education in emergency medicine is a lifelong journey, not a destination. We, as a program, will teach you the fundamental skills, knowledge and humanistic qualities that constitute the foundations of emergency medicine practice. Under the guidance and supervision of qualified faculty, residents need to develop a satisfactory level of clinical maturity, judgment and technical skill. Upon completion of this program, residents should be capable of practicing emergency medicine, be able to incorporate new skills and knowledge during their careers, and be able to monitor their own physical and mental well-being and that of others.
The Resident Education Committee has established specific educational and administrative criteria for promotion to the next program level and graduation from this program. Educational requirements are outlined for each program year in the “Educational Objectives” section in this handbook. Furthermore, ACGME core competencies criteria by which residents’ performance will be judged, is outlined in the “Evaluations” section in this handbook. Please read these over carefully.
Other promotion/graduation criteria include, but are not limited to:
- Procedure and Resuscitation log: Residents must document all procedures via the procedure tracking program online. All procedures and resuscitations must be put into the web-based procedure-tracking program. Remember to log every resuscitation in your online procedure log—the RRC thinks we do not do enough resuscitations. Procedure and resuscitation log review will be performed by the Residency Directors or faculty advisor at regular intervals and at your 6-month evaluation. One resuscitation per year must be logged in the competency-bot program. Please pay special attention to logging pediatric medical and trauma resuscitations and make sure to document your role in these resuscitations.
- Competency-bot: Every resident must complete 5 chief complaints per year in the online competency-bot program. You must also log 3 procedures and 1 resuscitation as competency procedures. One of these procedures must be an ultrasound. (Ultrasound guided central lines do not fulfill this requirement) This is an extensive evaluation where an attending must watch you perform the interview/procedure and fill out a form for all 9 of these competencies so please do not leave this to the last second. See the competency-bot section of the handbook for more info.
- Patient Care Follow-up: Residents will be required to keep online documentation of patient care and clinical questions encountered for EM patients. You must do 4 follow-ups per year and each one will require a lit review and an answer to some clinical question. You must complete 4 per year. No exceptions. These will be recorded in the Evaluations Manager online software. You may start them in the second block of each academic year when they are "opened."
- Six-month evaluation: Twice yearly the Residency Directors will review each resident’s performance and discuss progress, achievements, advancements, problems, and projects with the resident. Residents must fill out an extensive self–evaluation package prior to their six-month evaluation. This is obtained from the residency coordinator.
- Morning Report: All residents scheduled to work Monday, Tuesday, Thursday and Friday at KCHC at 7 AM or coming off the preceding overnight shift are required to attend. Residents scheduled at UHB are encouraged to attend at the discretion of the UHB Attending. Residents must first report to UHB for rounds and are to report back promptly at the conclusion of the case. The resident presenting the morning report is required to submit a one-page write-up to the residency coordinator for his/her Portfolio on each topic that he/she presents. The write-up should consist of a brief summary of the case with the pertinent teaching points highlighted.
- Wednesday conference attendance: The RRC mandates at least 70% conference attendance by all residents. Therefore, all residents are required to attend Wednesday conference, unless they are excused because of ACGME work hour requirements (see “Monthly Schedules” section in this handbook). Remember, you will already miss a significant portion of conference during vacation and off-service rotations. If you need to miss a conference, you must speak with one of the residency directors.
- USMLE Step 3: Passing Step III will be required by the end of your 2nd year in your residency training. You will be placed into a status called “non-renewal” if you do not have step 3 completed by the end of your second year. If you are still in “non-renewal” by the end of your third year, you will not be offered a contract to enter into your forth and final year of training and you will lose your spot in the residency. Do not take this lightly. It is hospital policy and not arguable.
- Summary of Resident portfolio: Residents are required to write a summary of their resident portfolio in order to be promoted to the next PGY level or to graduate. Please see the portfolio section of the handbook for more information
- Faculty advisor: Your faculty advisor should meet with you at least every 3 months. Although this will occur more or less frequently depending on the advisor, it is your responsibility to approach your advisor. Every meeting must be documented in the resident’s folder. There are Resident Evaluation Forms (see “Faculty Advisor” section of this handbook) that may be used as a guideline for resident-advisor meetings to address certain issues and to document regular meetings. This form must be given to the residency coordinator to be placed in the resident’s file. Please inform the Residency Directors if there are any problems with meeting with your advisor or if you wish to be assigned to a different advisor for any reason.
PLEASE BE AWARE: Compliance with the fulfillment of these regulations has been a problem in the past, especially during the last months of the final year. Please follow these rules carefully - it is ultimately the Program Director’s decision on whether to promote or graduate you.
Supervision of Residents and Escalation Policy
Residents working in the ED will be supervised by ABEM board-eligible or board certified attending physicians who are licensed in the state of their practice. When residents rotate on non-EM services, they will be supervised in accordance with the ACGME/RRC faculty supervision guidelines for that specialty. Residents rotating in the Pediatric Emergency Department may be supervised by faculty boarded or board-eligible in Pediatric Emergency Medicine.
Residents rotating in the Pediatric Emergency Department may also be immediately supervised by fellows enrolled in an ACGME-accredited Pediatric Emergency Medicine fellowship. However, these residents will also have immediate access to a faculty member who is board-certified/board-eligible in EM or Peds EM.
All EM residents are ultimately under the supervision of the Program Director of Emergency Medicine regardless of their present rotation.
In the ED, each patient encounter MUST be presented to a faculty member prior to disposition. All charts MUST be countersigned by an attending in a timely manner.
Junior residents can be supervised by senior residents in the ED or the respective specialty under which they are rotating, but they must ultimately be under a supervising faculty meeting the above criteria. Residents must be under direct supervision during all procedures until they are credentialed in that procedure. After that time, they will perform all procedures under general supervision. In the ED, there is always an attending in the clinical area to supervise all procedures. Faculty will not provide coverage from outside of the clinical area. As the residents progress in their level of training, they are given more autonomy in regards to patient management plans, procedures, and disposition.
Senior residents will be responsible for supervising the junior residents working in their assigned clinical area. Residents are also responsible for supervising and monitoring medical students. As residents progress, they may precept medical students. However, all patient encounters must ultimately be presented to the faculty in the clinical area. Residents will also work in conjunction with the nurse and clerical staff to assure that optimum patient care is given.
Further delineation of supervisory policies can be found in the resident handbook under that rotation summary.
POLICY ON RESIDENT WORK HOURS
Purpose:
To comply with New York Section Health Code Section 405 Regulations, ACGME Common Program Requirements and to establish a work environment with physicians fit for duty and conducive to resident/fellow education and the provision of safe and effective patient care. The following GME Committee policy has been accepted by the New York State Department of Health and conforms to NYSDOH Section 405 regulations and ACGME requirements revisions which became effective July 1, 2011.
Definitions:
Attending Physician: An appropriately privileged member of the medical staff who accepts full responsibility for a specific patient’s medical/surgical care.
Continuity clinic: Setting for a longitudinal experience in which residents develop a continuous, long-term therapeutic relationship with a panel of patients.
Duty Hours: time spent in all clinical and academic activities related to the program; i.e., patient care (both inpatient and outpatient), administrative duties relative to patient care, the provision for transfer of patient care, time spent in-house during call activities, and scheduled activities, such as conferences. Duty hours do not include reading and preparation time spent away from the duty site.
External moonlighting: Voluntary, compensated, medically-related work performed outside the institution where the resident is in training or at any of its related participating sites.
Faculty: Any individuals who have received a formal assignment to teach resident/fellow physicians. At some sites appointment to the medical staff of the hospital constitutes appointment to the faculty.
Fatigue management: Recognition by either a resident or supervisor of a level of resident fatigue that may adversely affect patient safety and enactment of a solution to mitigate the fatigue.
Fitness for duty: Mentally and physically able to effectively perform required duties and promote patient safety.
Night shift or night float: A duty assignment which takes place during night time hours and is distinct from on-call assignment.
On-Call: A period during which a resident is assigned to be in-house or available at home in addition to the regularly scheduled duty activities.
Residents or Fellows: Physicians engaged in a program of graduate medical education under the tutelage and supervision of appropriately qualified faculty and attending staff.
Scheduled duty periods: Assigned duty within the institution encompassing hours which may be within the normal work day, beyond the normal work day, or a combination of both.
Strategic napping: Short sleep periods, taken as a component of fatigue management, which can mitigate the adverse effects of sleep loss.
Transitions of care: The relaying of complete and accurate patient information between individuals or teams in transferring responsibility for patient care in the health care setting.
The ACGME Work Hours
(effective 7/1/2011)
Maximum Hours of Work per Week
Duty hours must be limited to 80 hours per week, averaged over a four- week period, inclusive of all in-house call activities and all moonlighting.
Duty Hour Exceptions
A Review Committee may grant exceptions for up to 10% or a maximum of 88 hours to individual programs based on a sound educational rationale.
Moonlighting
In preparing a request for an exception the program director must follow the duty hour exception policy from the ACGME Manual on Policies and Procedures.
Prior to submitting the request to the Review Committee, the program director must obtain approval of the institution’s GMEC and DIO.
Moonlighting must not interfere with the ability of the resident to achieve the goals and objectives of the educational program.
Time spent by residents in Internal and External Moonlighting (as defined in the ACGME Glossary of Terms) must be counted towards the 80-hour Maximum Weekly Hour Limit.
PGY-1 residents are not permitted to moonlight. Mandatory Time Free of Duty
Residents must be scheduled for a minimum of one day free of duty every week (when averaged over four weeks). At-home call cannot be assigned on these free days.
Maximum Duty Period Length
Duty periods of PGY-1 residents must not exceed 16 hours in duration.
Duty periods of PGY-2 residents and above may be scheduled to a maximum of 24 hours of continuous duty in the hospital. Programs must encourage residents to use alertness management strategies in the context of patient care responsibilities. Strategic napping, especially after 16 hours of continuous duty and between the hours of 10:00 p.m. and 8:00 a.m., is strongly suggested.
It is essential for patient safety and resident education that effective transitions in care occur. Residents may be allowed to remain on-site in order to accomplish these tasks; however, this period of time must be no longer than an additional four hours.
Residents must not be assigned additional clinical responsibilities after 24 hours of continuous in-house duty.
In unusual circumstances, residents, on their own initiative, may remain beyond their scheduled period of duty to continue to provide care to a single patient. Justifications for such extensions of duty are limited to reasons of required continuity for a severely ill or unstable patient, academic importance of the events transpiring, or humanistic attention to the needs of a patient or family.
Under those circumstances, the resident must:
- appropriately hand over the care of all other patients to the team responsible for their continuing care; and,
- document the reasons for remaining to care for the patient in question and submit that documentation in every circumstance to the program director.
The program director must review each submission of additional service, and track both individual resident and program-wide episodes of additional duty.
Minimum Time Off between Scheduled Duty Periods
PGY-1 residents should have 10 hours, and must have eight hours, free of duty between scheduled duty periods.
Intermediate-level residents [defined by the EM Review Committee as PGY2 residents] should have 10 hours free of duty, and must have eight hours between scheduled duty periods. They must have at least 14 hours free of duty after 24 hours of in-house duty.
Residents in the final years of education [defined by the EM Review Committee as PGY3 and 4 residents] must be prepared to enter the unsupervised practice of medicine and care for patients over irregular or extended periods.
This preparation must occur within the context of the 80- hour, maximum duty period length, and one-day-off-in- seven standards. While it is desirable that residents in their final years of education have eight hours free of duty between scheduled duty periods, there may be circumstances [as defined by the Review Committee] when these residents must stay on duty to care for their patients or return to the hospital with fewer than eight hours free of duty.
Circumstances of return-to-hospital activities with fewer than eight hours away from the hospital by residents in their final years of education must be monitored by the program director.
Maximum Frequency of In-House Night Float
Residents must not be scheduled for more than six consecutive nights of night float.
[The maximum number of consecutive weeks of night float, and maximum number of months of night float per year may be further specified by the EM Review Committee.]
Maximum In-House On-Call Frequency
PGY-2 residents and above must be scheduled for in-house call no more frequently than every-third-night (when averaged over a four-week period).
CLINICAL PROCEDURES
The purposes of procedure documentation are multiple. First, our program is required by the Resident Review Committee (RRC) section of the ACGME to ensure residents complete a certain number of procedures prior to completing their Emergency Medicine residency training. The RRC language is vague on the number of procedures required in most cases but is very strict about programs providing documentation of residents’ performing certain procedures. You will be supplied with a list of procedures that MUST be documented throughout your residency. This can be found on the log-in page of the New Innovations web site (www.new-innov.com) The other major reason for requiring documentation of residents’ procedures is that after completion of residency training, hiring institutions will require documentation of competence in certain procedures before Attending Physician privileges are granted. Over the last several years, many hospitals have become more rigorous with respect to verification of procedural competence during the credentialing process. Thus, it is important for the resident to receive credit for all procedures performed or supervised during training.
The SUNY-Downstate system has gone exclusively to web-based tracking of procedures and resuscitations. During your orientation you will be given information about how to log onto the New Innovations system to record your procedures.
Please realize that there are two different “requirements” for the number of procedures you will need to document. You will be given a purple procedure book that lists all of the major procedures we do in the ED and how many you must log before you are considered “credentialed” to do that procedure by yourself in the hospital without direct supervision. Once you are “officially credentialed by our hospital” to do that procedure, you will be able to perform that procedure without direct supervision at KCH and the other hospitals you rotate through. However, at that time, you may still need to log more of that procedure in order to meet the RRC’s expectations of how many procedures you must do in order to graduate from any EM residency program. Both of these sets of numbers are provided to you early in your residency.
Keeping an accurate record is not only important for your future employment credentialing process, but is also imperative to maintain our program’s RRC accreditation. Furthermore, keeping an updated procedure log is also part of your promotion/graduation requirements. If you have any problems or questions about the tracking program, please do not hesitate to contact Dr. Silverberg.
EVALUATIONS and FEEDBACK
Residents will be evaluated on each clinical and non-clinical rotation using the following evaluation & feedback mechanisms. The six (6) core competencies will be addressed in these evaluations as they apply to the individual rotation.
Evaluation process:
A. Resident Evaluation and Feedback
Multiple tools are used in the evaluation of the residents. They include oral feedback, written monthly evaluations, the EVALBOT computerized system, 6-month reviews with the Residency Directors, faculty advisor meetings, self-evaluation forms and a computerized SDOT (Standardized Direct Observational Tool), which is located on-line in the COMPOTENCYBOT computer program.
- Oral feedback is often provided by the supervising faculty during or after each clinical shift. If it is not, it should be sought.
- Brief written evaluation will be completed at the end of every rotation by supervising faculty and/or the Resident Education Committee. Additionally, the Residency Education Committee will fill out an in-depth evaluation on each resident at least twice per year to better pinpoint growth areas for each resident. These evaluations will can be found in New Innovations (NI) and can be reviewed at any time by the residents but must be signed prior to the resident completing their regular 6-month evaluations. When in the ED, Senior Residents will fill out electronic evaluation forms in NI for Junior Residents and vice versa, which will be reviewed by the Resident Education Committee. These evaluations are all open to review by the resident and faculty at all times. Residents review and sign all of these evaluations regularly but no less often than at their 6 month evaluations.(Next bullet)
- Twice yearly, one of the Residency Directors will review each resident’s performance and discuss progress, achievements, advancement, problems/concerns and projects with the individual resident.
- Residents must fill out an extensive self-evaluation package prior to each six-month evaluation.
- Residents are responsible to meet with their faculty advisor at least once quarterly for evaluation and feedback on performance. Advisors have full access and may look at their resident’s personal files including their portfolio, procedure certification and their “problems and concerns” file if any issues have been placed in this location.
- EVALBOT is a web-based computer program that allows all attendings to anonymously evaluate each resident as often as the individual attending likes. It can be daily after each shift working with a resident or whenever the EVALBOT program sends out a weekly reminder that certain residents are in the department. Each evaluation has 2 parts; first, the attending can submit any written comment that they want concerning the resident’s performance, skills or areas of concern. The second section is a 5-point scale used to rank the resident in each of the elements of the 6 core competencies.
- The COMPOTENCYBOT computer program requires direct observation by a faculty member in the clinical setting for approximately 10-20 minutes per encounter. The resident is required to get an attending to observe 5 patient interviews of different chief complaints, 3 procedures (including 1 sonogram) and 1 resuscitation each academic year. These numbers can be manually altered for certain residents that the Resident Education Committee feels needs to be evaluated more or less often than the general resident population. The goal is to evaluate the residents with specific attention paid to the elements of the 6 core competencies. Both faculty and resident are able to provide immediate feedback about that specific clinical encounter.
B. Follow ups:
- Residents will be required to keep electronic documentation of patient care follow-ups. This can include but is not limited to: ward/ICU visits with chart review, discussion with consultants who managed the patient after ED care, follow-up phone calls, procedure/operative/biopsy and autopsy reports and samples of discharge and transfer summaries. Each follow-up should conclude with a detailed search of the literature reviewing the pathology and pathophysiology surrounding each patient followed up and should also discuss the most up-to-date treatment guidelines found in the literature. The resident will be required to fill out one internet based in-depth follow up form 4 times per year. Our web-based computer program will keep track of how many each resident still needs to complete each academic year. This program is currently evaluations manager (www.sunyem.com/admin)
- Resident charts will be reviewed on a random basis as part of the Emergency Department’s ongoing Quality Assurance Program
C. Faculty Evaluation:
- All residents are required annually to evaluate all faculty members at KCH/Downstate and the affiliates using New Innovations. These evaluations are anonymous. This set of forms is electronically released at the start of block 7 to every resident for completion prior to May 15th. If you have not finished these evaluations prior to that May 15th date, you may not be eligible for promotion into the next year of residency including graduating from the program.
- Residents have the opportunity to evaluate faculty during their six month evaluation with the program directors as well
- The EVALBOT program can also be used to evaluate the attendings in an anonymous fashion similar to how the attendings evaluate the residents with comments. Residents will receive regular emails inviting them to evaluate faculty members.
D. Rotation Evaluation
- Residents must evaluate each of their rotations at the end of the block. Evaluations are done on line in New Innovations. They are generated each time a rotation ends. These forms will become part of the resident electronic file in New Innovations and will be reviewed by the program directors regularly.
E. Program Evaluation
- The program’s ability to achieve its stated goals and objectives is evaluated on a yearly basis by both faculty and residents through specially designed forms available from the residency coordinator.
PLEASE BE AWARE: Compliance with the fulfillment of these requirements has been a problem in the past. We will therefore deal with non-compliance very strictly. Residents in non-compliance will have to meet with one of the residency directors in person. They may be given extra assignments, have their clinical areas moved to undesirable locations or may even be prevented from advancing to the next year of their residency training (even graduating) if these goals have not been fulfilled.
RESIDENT PORTFOLIO
The resident portfolio is a useful tool to document all of your educational activities, assist you in the development of expertise and promotion, and will give you a sense of satisfaction and accomplishment. In addition, the portfolio will help you evaluate your own performance in a self-reflective manner.
This is the first step on your lifelong journey as a teacher and educator, and setting up your personal portfolio will help you gather and document all the educational activities throughout your career. At some point in your career you will have to present the same or similar information to your chairman when negotiating promotion and tenure as a faculty member.
There is a sample attached below.
The Portfolio should contain enough detail to allow evaluation of teaching and scholarly activity and yet be concise and selective as outlined. It should consist of two parts:
Part I: Summary - This is a summary of the teaching/scholarly activity documentation and should contain the following:
- A narrative statement (a teaching/scholarly activity philosophy):
This statement could be as short as one paragraph but shouldn’t exceed two single-spaced pages. It should include your clear goals, how you prepared to be an educator/researcher/administrator, what methods you used, what significant results you achieved, effective presentation of teaching materials, and reflective self-critique that allows you to improve.
It is not supposed to be an existential statement on your progress or your life; It intended to be based on the contents of your portfolio. It should indicate what you believe is important about your research/teaching/scholarly activity and how you put these believes into practice with specific regard to the five dimensions:
- Expertise in Content
- Instructional Design (what materials do you design to reach various types of learners, such as physician assistants, medical students, residents, fellows, attendings)
- Instructional Delivery (how do you communicate information to learners, i.e. lecture, workshop, facilitated discussion)
- Course Management Skills (how do you tell the learner how to be successful)
- Evidence of Student Learning (student/resident evaluations, passing exams, success of students/residents in their career, increased proficiency in examining and treating patients)
- A quantitative summary of teaching/scholarly activities:
This information may be presented in a summary format (sample provided as attachment).
Teaching/scholarly activities may include :
- formal didactic presentations (all lectures to faculty, seniors, juniors, medical students, journal club, CPC, Grand Rounds etc.)
- workshops (EKG/Radiology/Splinting workshop, ACLS, etc.)
- seminars
- panels
- informal discussions (focus group, topic review, literature battles, morning report, journal club, ultrasound teaching to juniors/students)
- advising/mentoring of medical students and residents
- teaching during clinical hours
- bedside teaching.
Other scholarly activities may include:
- research (grants, published research papers, abstracts, poster presentation)
- published articles
- textbook chapters
- editing journals/books
- written course material such as syllabi or outlines/handouts
- products of educational merit (videos, CD-ROM’s, computer based instruction, websites, exams)
- curriculum/courses designed/coordinated
- committee involvement/service activity
- educational courses attended (ACEP, SAEM, etc.)
- awards and honors
- evaluations (recommendation letters, lecture evaluation form, thank you letters)
Whenever possible, you should include proof of quality of teaching/scholarly activity including awards and evaluations or letters by faculty, peers, and medical students.
Part II: Appendices – Supporting documents for the Portfolio should be kept in a binder or folder documenting the activity, material produced and evaluation of the activity and material.
There are a few items you should include in your portfolio (some are in addition to the ones mentioned above):
- all printed and labeled ultrasound images
- one-page write up of your morning report
- lecture/journal club/presentation printouts, CD’s and/or handouts
- patient encounter follow up form (one per month)
- focus group questions and answers you prepared
- topic review questions and answers you prepared
PLEASE NOTE: The portfolio should be given to the residency coordinator and must be updated after every educational activity. It should be available and will be reviewed during the 6-months evaluation by the Residency Directors.
If you have any questions or need help, please contact the program director.
PORTFOLIO – SCHOLARLY ACTIVITIES WORKSHEET
- Teaching Awards and Honors
- Educational Committees
- Curricula Developed
- Lectures
- Workshops
- Seminars
- Panels
- Mentoring/Advisees
- Grants
- Research
- Publications
- Educational Materials Produced
- Educational Courses Attended
14. National Activities
|
Department of Emergency Medicine |
Memo
To: All EM and EM/IM Residents
From: Stephan Rinnert, MD
CC: Ms. Lane, Residency Directors
Re: Resident Portfolio Reflective Statement
As part of assessing the core competency in Problem based learning, all residents are required to maintain a resident portfolio in their resident file. This portfolio is supposed to catalog and demonstrate the resident’s academic achievement and prowess and is maintained and updated by the resident. The resident is solely responsible for content. The portfolio is kept by Ms. Lane, in your resident file.
If you have questions about the resident portfolio, please consult your handbook or Dr. Rinnert.
As part of your 6-month evaluation, you will be required to write a brief reflective statement based on the content of their portfolio. It can be in outline or narrative form but will be due with your 6-month self-assessment. Your 6-month self-assessment is not complete without the portfolio reflective statement.
I have attached references and a sample reflective statement for your reading pleasure
Please contact Dr. Rinnert with any questions.
Mathers NJ, Challis MC, Howe AC, Field NJ. Portfolios in continuing medical education--effective and efficient? Med Educ. 1999 Jul; 33(7):521-30.
Challis M, Mathers NJ, Howe AC, Field NJ. Portfolio-based learning: continuing medical education for general practitioners--a mid-point evaluation. Med Educ. 1997 Jan; 31(1):22-6.
Portfolio Reflective Statement
Dr. Rhubarb, EM PGY2
8/24/07
Upon review of my past year of academic work, I have come to the conclusion that my teaching activities are lacking but research activities are going VERY well.
While I completed the MICU conference and the Trauma conference as required, review of my MICU conference handout now shows it to be incomplete and uneven. I had a lot of information about dissection of the aorta but had only superficial coverage of aortic valvular catastrophes. This left the learner with an uneven review of the topic.
I was able to get 2 emedicine chapters published with Dr. Doty and both are now up on the web leaving me a total of 5 publications in 3 years. I have still not been able to get an original peer-reviewed RCT to be accepted for presentation but and actively working on the manuscript for “Glucose content in urine- A taste test to try.” With Dr. Rinnert and it look promising to be at least published in the NEJM as a lead article.
The patient follow-up are going well and I feel like I have a deeper understanding of the longitudinal care of the SLE patient with fever and patients with basilar skull fractures. I learned by doing that follow-up, that watchful waiting (as recommended by neurosurgery) for an expanding epidural hematoma is not optimal management and is often associated with poor outcomes.
I prepared 2 journal clubs that were well received and changed my practice in regards to managing NSTEMI patients.
Quality Improvement (QI) Project
SUNY Downstate / Kings County Hospital Emergency Medicine Residency Program
All residents in ACGME accredited residency programs are required to actively participate in emergency department continuous performance quality improvement programs. Residents must demonstrate evidence of development, implementation, and assessment of a project to improve care. This project may include but is not limited to the development of a clinical pathway, a patient satisfaction survey, or improvement of a recognized problem area. To ensure satisfaction of this requirement, all residents must complete the “Quality Improvement Project Form” which consists of two parts. The first part requires that the resident, under the supervision of a faculty project mentor, complete a proposal for a QI project by May 15th of their PGY3 year for categorical EM residents or PGY4 year for EM/IM residents. The second part requires that the resident complete their QI project by the end of their Administration rotation in their PGY4 year for categorical EM residents or PGY5 year for EM/IM residents. While the requirement may be fulfilled at anytime during the residency prior to the deadlines listed above (i.e. a QI research project or RIE completed during the PGY 2 year), both parts must be signed by the resident, project mentor, and the program director by the stated timeframes to satisfy completion of this residency requirement.
SUNY Downstate / Kings County Hospital Emergency Medicine Residency Program
Quality Improvement (QI) Project Form:
As a requirement of the RRC, all residents must complete a quality improvement project during their residency. This project must be found satisfactory by the program director or his/her designee. In order to verify completion of this requirement, both parts 1 and 2 of this form must be submitted by the stated timeframes.
Part 1: QI project proposal – Must be completed before May 15th of your PGY3 year for categorical EM residents or PGY4 year for EM/IM residents.
Resident Name: ______________________________________________________________________________
Project Mentor: ______________________________________________________________________________
Title of project: ______________________________________________________________________________
Description of proposed project: _____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
This proposal satisfies Part 1 of the residency requirement for involvement in a quality improvement project.
_________________________________________________ ________________________________________
Resident Signature Date
_________________________________________________ ________________________________________
Project Mentor Signature Date
_________________________________________________ ________________________________________
Program Director Signature Date
Part 2: QI project completion – Must be completed before the end of the Administration rotation of your PGY4 year for categorical EM residents or PGY5 year for EM/IM residents.
Resident Name: ______________________________________________________________________________
Project Mentor: ______________________________________________________________________________
Summary of completed project: _____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Date of QI project completion: ______________________________________________________________
This project satisfies Part 2 of the residency requirement for participation in a quality improvement project.
_________________________________________________ ________________________________________
Resident Signature Date
_________________________________________________ ________________________________________
Project Mentor Signature Date
_________________________________________________ ________________________________________
Program Director Signature Date
Pay line switching
You may want to switch your pay source during your residency. This is allowed but must follow these rules.
- Interns are placed on lines as we need them. They don’t get a choice.
- Once on a pay line, you will never HAVE to switch your pay line if you don't want to. Switching may affect your other benefits and you are not forced to do that.
- If you want to switch your pay source, then you need to put it in writing and send to me by March 1st of the year you wish to switch. (we switch each July)
- Once you ask to be moved, there is no switching again. You will be on that pay line until you are complete with residency. You get one shot at this.
- You may be asked to switch your pay line for the benefit or equity or the program. If you refuse then you can stay on your present line. However, you will have to stay on that line until you have completed your residency.
Please note:
The Program Director has final say to amend or revoke any of these rules if they feel it is in the best interest of the entire program.
TRAVEL PLANS & REIMBURSEMENT PROCEDURES
The following outlines the procedure to follow regarding travel/conference reimbursements.
- Complete travel approval request form prior to the event and return to Martha Patella for approval by Residency Director, Chairman and/or Dean.
a. Attach documentation legitimizing conference. i.e. front page of the brochure or blank registration form.
b. This is for any type of travel that you anticipate getting reimbursed for.
When in doubt, ask Ms. Patella prior to the event.
You do not have to have definitive plans to submit a request. This process can take 3 months so if you are considering any type of travel submit the request as early as possible. You are not making a commitment, just a request.
- Once you receive the approval notice(again this can take 3 months)see Ms. Patella to make airline/rail reservations, through the SUNY travel agent. There will be no out of pocket for airlines or rail travel. It will be paid directly through SUNY. (Please note that you will not be reimbursed should you book and pay for your air/rail travel on your own.)
3. After you receive the approval notice, you can register and pay for conferences and hotel reservations. After the conference bring your original receipts to Ms. Patella and complete a travel voucher form. SUNY will reimburse directly to your home. They will also reimburse for cab fare, breakfast and dinner (no lunch) only with original legible, itemized receipts. If you intend to rent a car, a letter justifying the expense will be required.
GME Due Process Policy
SUNY Downstate Medical Center
Graduate Medical Education
Purpose:
To establish a policy for all post-graduate medical programs of SUNY Downstate Medical Center for use in addressing all actions that can result in altering the intended career path of a resident or fellow. To provide residents and fellows with fair, reasonable and readily available policies and procedures for grievance and due process through a decision-making process while minimizing conflict of interest by adjudicating parties.
Scope:
This policy applies to all programs and house officers (residents and fellows) participating in graduate medical education programs sponsored by SUNY Downstate. This policy applies to actions taken as a result of academic deficiencies or misconduct.
Definitions:
Due Process: an individual’s right to be adequately notified of any changes or proceedings involving him or her, and the opportunity to be meaningfully heard with respect to those proceedings.
House Staff or House Officer: refers to all interns, residents or fellows enrolled in post-graduate medical training or research program or activity
GME Program: refers to a residency or fellowship educational program
Adverse Action: disciplinary actions taken against a resident which alter the intended career development or timeframe. Such actions are reportable and allow a request for review and due process Adverse actions include the following:
Dismissal: act of terminating a house officer participating in a GME program prior to successful completion of the course of training whether by early termination of a contract or by non-renewal of a contract.
Non-renewal: act of not reappointing a house officer to subsequent years of training prior to fulfillment of a complete course of training.
Non-promotion: act of not advancing a house officer to the next level of training according to the usual progression through a program
Extension of Training: act of extending the duration of time required by a house officer to complete a course of training generally resulting from repeating unsatisfactory rotation assignments or remediating poor performance or needing additional time to demonstrate achievement of required competence in one or more domains.
Probation: placement of a resident under close monitoring for specific performance concerns which if not successful resolved may result in other adverse actions including dismissal. This action is reportable to state licensing authorities and health care institutions.
Suspension: Withdrawal of privileges for participating in clinical, didactic or research activities associated with appointment to the training program or hospital staff. This action is taken if, in the judgment of the Program Director, Department Chairperson or institutional leadership (Associate Dean, Dean, Medical Director) a resident’s or fellow’s competence or behavior is such that patients may be endangered, the educational process disrupted or other peers, staff, faculty are subjected to an adverse and unacceptable work environment. Under such circumstances, suspension may be implemented immediately pending further investigation and determination of other appropriate action. Suspension may be with salary or salary may be withheld after consultation with the labor relations department of the employing facility.
Policy:
Academic Matters:
The SUNY Downstate GME Academic Performance Policy affords due process to residents/fellows who are subject to adverse actions or whose intended career development is altered by an academic decision of a program. See Academic Performance Policy for delineation of specific processes provided.
Misconduct Matters:
The SUNY Downstate Resident/Fellow GME Misconduct Policy affords due process to residents/fellows who are subject to adverse actions or dismissed from a GME program in a manner that alters their intended career development. See Resident/Fellow GME Misconduct Policy for delineation of specific processes provided.
Policy revised and updated on 5/13/2011. This Policy supersedes all prior, similar and/or related versions and revisions. Revisions approved by GMEC 5/18/11. Effective immediately upon approval.
GME Academic Performance Due Process Policy
SUNY Downstate Medical Center
Graduate Medical Education
Purpose:
To establish a policy and procedure for all post-graduate medical programs of SUNY Downstate Medical Center to use in addressing deficiencies in the academic performance, competence or progress of a resident or fellow enrolled in a graduate medical education program. To provide fair, reasonable and readily available policies and procedures when a resident/fellow is not meeting the academic expectations of a program or fails to progress.
Scope:
This policy applies to all programs and house officers (residents and fellows) participating in graduate medical education programs sponsored by SUNY Downstate. This policy applies to actions taken as a result of academic deficiencies that may involve the knowledge, skills, attitudes or the core clinical competencies of medical knowledge, patient care, systems-based practice, practice-based learning and improvement, communications and interpersonal skills and aspects of professionalism which are not addressed by the GME Misconduct Policy. This policy describes minimum expectations providing residents with an opportunity to be notified of deficiencies and an opportunity to cure those deficiencies.
Definitions:
Due Process: an individual’s right to be adequately notified of any changes or proceedings involving him or her, and the opportunity to be meaningfully heard with respect to those proceedings.
House Staff or House Officer: refers to all interns, residents or fellows enrolled in post-graduate medical training or research program or activity. The terms house officer, house staff, residents, fellows or subspecialty residents or fellows may be used interchangeably.
GME Program: refers to a residency or fellowship educational program
Letter of Deficiency: a non-reportable warning issued to a resident/fellow when there are concerns that routine feedback is not effecting necessary improvement. Such a letter provides the house officer with formal notice and opportunity to cure any deficiencies. The Program Director can choose to alter a resident’s assignments or have a resident repeat rotation(s) or make other adjustments in the resident’s program in order to provide opportunity to cure the deficiency. It is an academic notification which is not reported to outside agencies and is not subject to appeal or review. The letter should summarize deficiencies and may identify expectations for demonstrating improvement as well as the consequences of not successfully resolving the deficiencies. Copies of Letters of Deficiency, signed and dated by the Program Director, should be retained in the resident’s training record with copies to the GME Office. It is advisable to have the resident indicate receipt of Letters of Deficiency by signature or by witness or other documentation. These letters are sometimes also referred to as “Letter of Warning.”
Monitored Performance: an academic function involving a heightened level of monitoring and assessment of house officer performance in the course of training program activities usually used to further assess for improvement in noted areas of deficiency, often as part of a program for remediation. This is not an adverse action, not reportable and not subject to appeal.
Adverse Action: disciplinary actions taken against a resident which alter the intended career development or timeframe. Such actions are reportable and allow a request for review and due process. Adverse actions include the following:
Dismissal: act of terminating a house officer participating in a GME program prior to successful completion of the course of training whether by early termination of a contract or by non-renewal of a contract.
Non-renewal: act of not reappointing a house officer to subsequent years of training prior to fulfillment of a complete course of training.
Non-promotion: act of not advancing a house officer to the next level of training according to the usual progression through a program
Extension of Training: act of extending the duration of time required by a house officer to complete a course of training generally resulting from repeating unsatisfactory rotation assignments or remediating poor performance or needing additional time to demonstrate achievement of required competence in one or more domains.
Probation: placement of a resident under close monitoring for specific performance concerns which if not successfully resolved can result in further adverse actions including dismissal. This action is reportable to state licensing authorities, employers and health care institutions.
Suspension: withdrawal of privileges for participating in clinical, didactic or research activities associated with appointment to the training program or hospital staff. This action is taken if, in the judgment of the Program Director, Department Chairperson or institutional leadership (Associate Dean, Dean, Medical Director) a resident’s or fellow’s competence or behavior is such that patients may be endangered, the educational process disrupted or other peers, staff, faculty are subjected to an adverse and unacceptable work environment. Under such circumstances, suspension may be implemented immediately pending further investigation and determination of other appropriate action. Suspension may be with salary or salary may be withheld after consultation with the labor relations department of the employing facility.
Structured Feedback: routine feedback regarding a trainee’s performance or behavior and consistent with the educational program. Structured feedback can consist of verbal feedback, rotational and summative evaluations, spontaneous or “on-the-fly” formal evaluations, memos or letters to a resident’s record or to the Program Director and shared with the resident, discussion and recommendations of a Program’s Clinical Competence or Resident Performance or other similar committee.
Policy:
All programs must establish a process for evaluating residents consistent with sound andragogic practice, ACGME institutional, common program and specialty specific requirements, American Board of Medical Specialties specialty board specific requirements and those of any other agency or accrediting body. Assessment of house officer performance and competence is made based upon department, program and/or specialty-specific educational requirements and expectations.
All residents and fellows should be provided with routine structured feedback that is consistent with the educational program and its policies.
Each department should establish a committee of faculty who meet regularly, no less frequent than four times per year, to review the performance, competence and/or standing in the program and progress toward program completion for all enrolled residents. This committee which may be referred to as a Clinical Competence Committee (CCC) or Performance or Evaluation Review Committee or House Staff Affairs or Assessment Committee, for example, should provide recommendations to the Program Director regarding the status of residents in the program and their progress to advanced training levels and, ultimately, program completion. The Committee’s discussions should be documented in meeting minutes. A Department can have one committee that reviews all residents and fellows in all programs in that Department. Alternatively, for Departments with multiple programs, residencies and fellowships, there may be separate and independent committees for each program. However, there must me no more than one committee with responsibility for assessing progress of all residents in a program and perspective on how all the program’s residents are performing relative to one another and longitudinally in time.
Letter of Deficiency: When a resident or fellow has been identified as having deficiency, it is expected that he/she will receive routine structured feedback in order to identify and correct the issue. When the Program Director and/or CCC deems that routine feedback is not effecting necessary improvements, or if the Program Director and/or CCC determines that the deficiency is significant enough to warrant more than routine feedback, the Program Director and/or CCC may elect to issue a “Letter of Deficiency.” This letter formally provides the House Officer with (a) notice of the deficiency and (b) an opportunity to cure the deficiency. “Letters of Deficiency” must be signed and dated by the Program Director and copied to the resident/fellow’s record and to the GME Office. The “Letter of Deficiency” must indicate the possible outcomes of failure to fully resolve the concerns or developing deficiencies or performance problems in additional areas. The issuance of a “Letter of Deficiency” does not trigger a report to any outside agencies. The House Staff Officer should continue to receive structured feedback addressing issues consistent with the “Letter of Deficiency.” The house officer may be subjected to a period of monitored performance to appropriately assess progress in resolving deficiencies. If the house officer satisfactorily resolves deficiencies noted in the “Letter of Deficiency,” and continues to perform acceptably thereafter, the period of unacceptable academic performance does not affect the house officer’s intended career development.
Escalation: If the Program Director and/or CCC determine that the house officer has failed to satisfactorily cure the deficiency and/or improve his/her performance to an expected and acceptable level, with consideration for what is fair and reasonable, the Program Director and/or CCC may elect to take further actions. Such actions may include but are not limited to any one or more of the following:
- Issuance of another, new “Letter of Deficiency.” (Non-reportable, not an adverse action)
- Placement on probation with establishment of adverse consequences for unsuccessfully meeting conditions of the probation
- Non-promotion to the next PGY or training level and continue in the program.
- Require repeat of training experience that in turn results in extension of required period of training
- Extension of contract which may involve extension of the defined training period (extension of training)
- Denial of credit for previously completed rotations/experiences
- Non-renewal in the training program
- Suspension from training pending further review or determination of other definitive action.
- Dismissal from the residency or fellowship program.
For all such actions, the resident must be notified verbally, when possible, and in writing. A copy of the notification signed and dated by the Program Director with documentation that it was received by the resident (resident signed acknowledgement or witnessed or other receipt verification) must be included in the resident’s record and copied to the GME Office. Notice of adverse action or any action which can interfere with the resident’s intended career development must inform the house officer of his/her right to review and appeal of such adverse action. The house officer should be provided with or referred to applicable policies and procedures regarding due process, review and appeal. Notifications of adverse action should be done in consultation with the GME Office.
Reportable Actions: The decision not to promote a house officer to the next PGY level, to extend training, to deny credit for a period of training, suspension, probation, and/or terminating a house officer’s participation in a residency or fellowship program are each considered “reportable actions.” Such actions must be disclosed to others upon request, including without limitation, future employers, privileging hospitals, and licensing and specialty boards. House Officers who are subject to a reportable action are permitted to request a review of the decision and seek to appeal that decision. Note that routine academic performance evaluations and assessments even when unsatisfactory are standard procedures in a training program and in and of themselves are not considered adverse actions, are not reportable actions and are not subject to appeal under this policy.
Request for Review and Appeal: A review and appeal of a Program’s decision to take a Reportable Action or any action interfering with the resident’s intended career development may be requested by the house officer. The request must be made in writing, addressed to the Associate Dean for GME, signed and dated, and submitted to the Director of Graduate Medical Education within 14 calendar days of the house officer learning of the Reportable Action. The request should clearly describe the reason for requesting the review and any basis upon which an appeal is being made. Upon receipt of a Request for Review and Appeal, the Associate Dean for GME will determine whether the matter is subject to review under this Policy. If so, the Associate Dean for GME will direct the Director of GME to appoint an ad hoc Review and Appeal Subcommittee of the GME Committee. This subcommittee will be composed of neutral reviewers from Departments other than the one in which the requesting house officer is appointed. The subcommittee will consist of at least two SUNY Downstate faculty members and one resident or fellow. Additional committee members may be assigned at the discretion of the Associate Dean for GME/DIO. The subcommittee may also include institutional GME Department leadership such as the Vice Dean for GME, Associate Dean for GME, the DIO or GME Office administrative officers. SUNY Counsel may serve in an advisory capacity.
The ad hoc Review and Appeal subcommittee will:
- Conduct confidential meeting(s) open only to committee members, GME Office and GMEC staff, and any participants invited by and approved by the Committee.
- Identify one faculty member who will serve as Chairperson of the subcommittee. The subcommittee Chairperson should be a participant on the SUNY Downstate GME Committee.
- Arrange for an individual to take notes and document a summary of minutes of meetings held.
- Committee meetings will be scheduled at the discretion of the committee Chairperson.
- Establish a process for the review. Such process will not be rigidly prescribed and is not conducted in the manner of a legal hearing process. No legal representation will be permitted. No opportunity for cross examination or questioning is offered.
- Review the resident/fellow complaint and request for review/appeal.
- Provide the house officer requesting the review or appeal the opportunity to appear before the committee to make a statement and/or present evidence of relevance for rescinding the action under review. The committee may also require the house officer to respond to questions posed by the committee. As an academic review panel and not a legal hearing, when appearing before the committee, the house officer may be accompanied by an advocate who is not an attorney. Failure of an appealing house officer to appear as scheduled before the committee without just cause could result in a summary determination against the house officer.
- If applicable, review relevant records and documentation such as the house officer’s file, program records, policies, meeting minutes, etc.
- Consider any extenuating circumstances.
- The committee may meet with the Program Director or other program representative(s) and request presentation of evidence for upholding the proposed action.
- The committee may request statements from or interview other house officers, faculty, staff, administrators or members of the academic or health care team in order to gather additional information.
- The committee may consult with others, as appropriate, to assist in the decision making process.
- Determine whether this Policy was followed, the house officer received notice and an opportunity to cure, and the decision to take the reportable action was reasonably made.
- The subcommittee Chairperson is responsible for preparing the committee’s report summarizing findings and making recommendations to the Associate Dean for GME/DIO regarding the review and request for appeal of reportable actions.
- The subcommittee Chairperson or designee will report the outcome of the review and appeal process to the GME Committee.
Upon receipt of the Chairperson’s report from the ad hoc Review and Appeal Subcommittee, the Associate Dean for GME shall review said findings and recommendations. The Associate Dean for GME/DIO finding the committee’s review process to have followed procedure and be fair, reasonable and appropriate shall make notification to the resident of the Review and Appeal subcommittee’s decision in writing with a copy to the Program Director, Department Chairperson, the employing institution, if applicable, and others as appropriate.
The decision resulting from this review is a final and binding decision. It is not subject to further formal review within the State University of New York Downstate Medical Center (Health Science Center at Brooklyn).
No Retaliation: Initial and full inquiries will be conducted with due regard for confidentiality to the extent practicable. Under no circumstances may anyone retaliate against, interfere with or discourage anyone from participating in good faith in an initial inquiry or full inquiry conducted under this policy. A house staff officer who believes he/she may have been retaliated against in violation of this policy should immediately report it to his/her supervisor, the Director of GME, resident ombudsman, Associate Dean for GME, DIO or other any other supervisor.
Original policy completed on 5/13/2011. This Policy supersedes all prior, similar and/or related versions and revisions. Reviewed and approved by GMEC May 18, 2011. Effective immediately upon approval.
GME Misconduct Due Process Policy
SUNY Downstate Medical Center
Graduate Medical Education
Purpose:
To establish a policy and procedure for all post-graduate medical programs of SUNY Downstate Medical Center to use in addressing allegations of misconduct made against a house staff officer. To provide fair, reasonable and readily available policies and procedures regarding charges of misconduct.
Scope:
This policy applies to all programs and house officers (residents and fellows) participating in graduate medical education programs sponsored by SUNY Downstate. This policy applies to any actions taken as a result of allegations of misconduct or serious departure from standards of professionalism or professional expectations. This policy describes minimum expectations providing residents with an opportunity to be notified of allegations and an opportunity to be heard and respond to such allegations and any proposed action taken as a result.
Definitions:
Due Process: an individual’s right to be adequately notified of any changes or proceedings involving him or her, and the opportunity to be meaningfully heard with respect to those proceedings.
House Staff or House Officer: refers to all interns, residents or fellows enrolled in post-graduate medical training or research program or activity at SUNY Downstate or as a visiting rotator to SUNY Downstate.
GME Program: refers to a structured educational experience in graduate medical education designed to conform to the Program Requirements of a particular specialty/subspecialty
Misconduct: refers to improper behavior; intentional wrongdoing; violation of law, rule, standard of practice, or policy of the program, department, institution or agency including NYS Education Law Section 6530 (synopsis attached as appendix 1). Misconduct may also constitute unprofessional behavior, which may also trigger action under the GME Academic Deficiencies Policy, not to the exclusion of any action resulting from this GME Misconduct Policy. These actions may proceed simultaneously.
Monitored Performance: an academic function involving the heightened level of monitoring and assessment of house officer performance in the course of training program activities usually used to further assess for improvement in noted areas of deficiency, often as a part of a program for remediation. This is not an adverse action and it is not reportable.
Adverse Action: disciplinary actions taken against a resident which alter the intended career development or timeframe. Such actions are reportable and allow a request for review and due process. Adverse actions include the following:
Dismissal: act of terminating a house officer participating in a GME program prior to successful completion of the course of training whether by early termination of a contract or by non-renewal of a contract.
Non-renewal: act of not reappointing a house officer to subsequent years of training prior to fulfillment of a complete course of training.
Non-promotion: act of not advancing a house officer to the next level of training according to the usual progression through a program.
Extension of Training: act of extending the duration of time required by a house officer to complete a course of training generally resulting from repeating unsatisfactory rotation assignments or remediating poor performance or needing additional time to demonstrate achievement of required competence in one or more domains.
Probation: placement of a resident under close monitoring for specific performance concerns which if not successfully resolved may result in other adverse actions including dismissal. This action is reportable to state licensing authorities and health care institutions.
Suspension: withdrawal of privileges for participating in clinical, didactic or research activities associated with appointment to the training program or hospital staff. This action is taken if, in the judgment of the Program Director, Department Chairperson or institutional leadership (Associate Dean, Dean, Medical Director) a resident’s or fellow’s competence or behavior is such that patients may be endangered, the educational process disrupted or other peers, staff, faculty are subjected to an adverse and unacceptable work environment. Under such circumstances, suspension may be implemented immediately pending further investigation and determination of other appropriate action. Suspension may be with salary or salary may be withheld after consultation with the labor relations department of the employing facility.
Structured Feedback: routine feedback regarding a trainee’s performance or behavior and consistent with the educational program. Structured feedback can consist of verbal feedback, rotational and summative evaluations, spontaneous or “on-the-fly” formal evaluations, memos or letters to a resident’s record or to the Program Director and shared with the resident, discussion and recommendations of a Program’s Clinical Competence or Resident Performance or other similar committee.
Policy:
A house officer, employee of the hospital, attending physician, patient, or any other person who believes that a house officer has engaged in misconduct of any kind should immediately report his/her concern to his/her supervisor, or any other supervisor in the institution, who in turn should communicate the allegations to the house officer’s Program Director. Upon receipt of a complaint regarding the conduct of a house officer, the Program Director should conduct an initial inquiry, as follows:
- Review documentation of and in support of the complaint
- If possible, meet with the person complaining of misconduct
- Meet with the house officer to advise the house officer of the existence of the complaint, to notify him or her and provide an opportunity to respond to the allegations, and to identify any potential witnesses or other information relevant to the alleged misconduct
- Consult with GME Office to determine whether the Dean, Associate Dean for GME, Department Chairperson, Legal Affairs and/or Human Resources and/or Labor Relations should be contacted as appropriate based on the issues and the people involved
- Upon the request of the house officer, or if the Program Director, Associate Dean for GME/DIO, Department Chairperson or Human Resources decide the incident warrants more investigation, then a “Full Inquiry” must be done
- All allegations of sexual harassment, disruptive behavior or violence must be reported to Human Resources/Labor Relations in accordance with the Institution’s policies.
- Upon consensus of the Program Director and the Associate Dean for GME/DIO or designee, the accused house staff officer can be removed from duty (with or without pay) pending the outcome of a full inquiry
Full Inquiry:
A full inquiry is an internal investigation of the allegations/incident by a committee of appropriate individuals appointed by the Department Chairperson from within the Department/Institution. This may include GME staff or leadership, Program Director, Department Chairperson, key faculty, Human Resources, Legal Affairs, Labor Relations, Hospital Administration, or others. The inquiry process is administered by the Department Chairperson in consultation with the GME Office. Factual results of the inquiry along with recommendations for action will be prepared by the Chairperson and/or other responsible faculty or staff participating in the full inquiry and reported back to the Program Director and the house officer for appropriate action. A copy of this report will be submitted to the GME Office and Associate Dean for GME/DIO. If the full inquiry results in a finding that no misconduct occurred, no action will be taken against the house officer. If the house officer was suspended pending the inquiry, the house officer will be reinstated with full benefits and pay without prejudice. If the full inquiry results in a finding that the house officer engaged in misconduct, the Program Director shall determine, in consultation with the Department Chair, Human Resources, Legal Affairs, Labor Relations or other appropriate individuals, what action is appropriate under the circumstances, to remedy the situation. At all times, quality of patient care, safety of patients, staff, faculty and house officers, and integrity and security of the work and education environment must be assured. The Program may take actions including, without limitation, the following:
- Verbal or written warning or reprimand.
- Election to not promote to the next training level.
- Non-renewal of contract.
- Suspension.
- Probation.
- Immediate termination or dismissal from residency or fellowship program.
Reportable Actions: The decision not to promote a house officer to the next PGY level, to extend training, to deny credit for a previously completed period of training, suspension, probation, and/or terminating a house officer’s participation in a residency or fellowship program are each considered “reportable actions.” Such actions must be disclosed to others upon request, including without limitation, future employers, privileging hospitals, and licensing and specialty boards. House Officers who are subject to a reportable action are permitted to request a review of the decision and seek to appeal that decision.
For all such actions, the resident must be notified verbally, when possible, and in writing. A copy of the notification signed and dated by the Program Director with documentation that it was received by the resident (resident signed acknowledgement or witnessed or other receipt verification) must be included in the resident’s record and copied to the GME Office. Notice of adverse action or any action which can interfere with the resident’s intended career development must inform the house officer of his/her right to review and appeal of such adverse action. The house officer should be provided with or referred to applicable policies and procedures regarding due process, review and appeal. Notifications of adverse action should be done in consultation with the GME Office. Note that performance evaluations and assessments, even when unsatisfactory, are standard procedures in a training program and in and of themselves are not considered adverse actions, are not reportable actions and are not subject to appeal under this policy. Verbal or written warnings and/or reprimands are also not considered adverse actions, are not reportable and are not subject to appeal under this policy.
Request for Review and Appeal:
A review and appeal of a Program’s decision to take a Reportable Action or any action interfering with the resident’s intended career development may be requested by the house officer. The request must be made in writing, addressed to the Associate Dean for GME, signed and dated, and submitted to the Director of Graduate Medical Education within 14 calendar days of the house officer learning of the Reportable Action. The request should clearly describe the reason for requesting the review and any basis upon which an appeal is being made. Upon receipt of a Request for Review and Appeal, the Associate Dean for GME will determine whether the matter is subject to review under this Policy. If so, the Associate Dean for GME will direct the Director of GME to appoint an ad hoc Review and Appeal Subcommittee of the GME Committee. This subcommittee will be composed of neutral reviewers from Departments other than the one in which the requesting house officer is appointed. The subcommittee will consist of at least two SUNY Downstate faculty members and one resident or fellow. Additional committee members may be assigned at the discretion of the Associate Dean for GME/DIO. The subcommittee may also include institutional GME Department leadership such as the Vice Dean for GME, Associate Dean for GME, the DIO or GME Office administrative officers. SUNY Counsel may serve in an advisory capacity.
The ad hoc Review and Appeal subcommittee will:
- Conduct confidential meeting(s) open only to committee members, GME Office and GMEC staff, and any participants invited by and approved by the Committee.
- Identify one faculty member who will serve as Chairperson of the subcommittee. The subcommittee Chairperson should be a participant on the SUNY Downstate GME Committee.
- Arrange for an individual to take notes and document a summary of minutes of meetings held.
- Committee meetings will be scheduled at the discretion of the committee Chairperson.
- Establish a process for the review. Such process will not be rigidly prescribed and is not conducted in the manner of a legal hearing process. No legal representation will be permitted. No opportunity for cross examination or questioning is offered.
- Review the resident/fellow complaint and request for review/appeal.
- Provide the house officer requesting the review or appeal the opportunity to appear before the committee to make a statement and/or present evidence of relevance for rescinding the action under review. The committee may also require the house officer to respond to questions posed by the committee. As an academic review panel and not a legal hearing, when appearing before the committee, the house officer may be accompanied by an advocate who is not an attorney. Failure of an appealing house officer to appear as scheduled before the committee without just cause could result in a summary determination against the house officer.
- If applicable, review relevant records and documentation such as the house officer’s file, program records, policies, meeting minutes, etc.
- Consider any extenuating circumstances.
- The committee may meet with the Program Director or other program representative(s) and request presentation of evidence for upholding the proposed action.
- The committee may request statements from or interview other house officers, faculty, staff, administrators or members of the academic or health care team in order to gather additional information.
- The committee may consult with others, as appropriate, to assist in the decision making process.
- Determine whether this Policy was followed, the house officer received notice and an opportunity to be heard, and the decision to take the reportable action was reasonably made.
- The subcommittee Chairperson is responsible for preparing the committee’s report summarizing findings and making recommendations to the Associate Dean for GME/DIO regarding the review and request for appeal of reportable actions.
- The subcommittee Chairperson or designee will report the outcome of the review and appeal process to the GME Committee.
Upon receipt of the Chairperson’s report from the ad hoc Review and Appeal Subcommittee, the Associate Dean for GME shall review said findings and recommendations. The Associate Dean for GME/DIO finding the committee’s review process to have followed procedure and be fair, reasonable and appropriate shall make notification to the resident of the Review and Appeal subcommittee’s decision in writing with a copy to the Program Director, Department Chairperson, the employing institution, if applicable, and others as appropriate.
The decision resulting from this review is a final and binding decision. It is not subject to further formal review within the State University of New York Downstate Medical Center (Health Science Center at Brooklyn).
No Retaliation: Initial and full inquiries will be conducted with due regard for confidentiality to the extent practicable. Under no circumstances may anyone retaliate against, interfere with or discourage anyone from participating in good faith in an initial inquiry or full inquiry conducted under this policy. A house staff officer who believes he/she may have been retaliated against in violation of this policy should immediately report it to his/her supervisor, the Director of GME, resident ombudsman, Associate Dean for GME, DIO or other any other supervisor.
Original policy completed on 5/13/2011. This Policy supersedes all prior, similar and/or related versions and revisions. Reviewed and approved by GMEC 5/18/11. Effective immediately upon approval.
Appendix 1:
Synopsis of NYS Education Law Section 6530
- Obtaining a license or permit fraudulently;
- Practicing the profession fraudulently or beyond its authorized scope;
- Practicing the profession with gross negligence on a particular occasion or negligence on more than one occasion;
- Practicing the profession with gross incompetence or incompetence on more than one occasion;
- Practicing the profession while impaired by alcohol, drugs, physical disability, or mental disability;
- Being a habitual abuser of alcohol, or being dependent on or a habitual user of narcotics, barbiturates, amphetamines, hallucinogens, or other drugs having similar effects, except if maintained on an approved therapeutic regimen which does not impair the ability to practice;
- Having a psychiatric condition which impairs the ability to practice;
- Being convicted of committing an act constituting a crime under New York State law, federal law or another jurisdiction which, if committed within New York State, would have constituted a crime under New York law;
- Refusing to provide professional service to a person because of such person’s race, creed, color or national origin;
- Permitting, aiding or abetting an unlicensed person to perform activities requiring a license;
- Any willful violation of New York State Public Health Law or Education Law or Public Officers Law;
- A willful of grossly negligent failure to comply with substantial provisions of federal, state, or local laws, rules, or regulations governing the practice of medicine;
- Exercise undue influence on the patient in such a manner as to exploit the patient for financial gain;
- Directly or indirectly offering, giving, soliciting, or receiving or agreeing to receive, any fee or other consideration to or from a third party for the referral of a patient or in connection with the performance of professional services;
- Conduct in the practice of medicine which evidences moral unfitness to practice medicine;
- Willfully making or filing a false report, or failing to file a report required by law or by the Department of Health or the Education Department, or willfully impeding or obstructing such filing, or inducing another person to do so;
- Revealing of personally identifiable facts, data, or information obtained in a professional capacity without the prior consent of the patient, except as authorized or required by law;
- Practicing or offering to practice beyond the scope permitted by law, or accepting and performing professional responsibilities which the physician knows or has reason to know that he or she is not competent to perform, or performing without adequate supervision professional services which the physician is authorized to perform only under the supervision of a licensed or appropriate privileged professional, except in an emergency situation where a person’s life or health are in danger;
- Delegating professional responsibilities to a person while knowing or having reason to know that such person is not qualified, by training, by experience, or by licensure, to perform them;
- Performing professional services which have not been duly authorized by the patient or his or her legal representative;
- Abandoning or neglecting a patient under and in need of immediate professional care, without making reasonable arrangements for the continuation of such care, or abandoning a professional employment without reasonable notice and under circumstances which seriously impair the delivery of professional care to patients or clients;
- Willfully harassing, abusing, or intimidating a patient either physically or verbally;
- Failure to maintain a record for each patient which accurately reflects the evaluation and treatment of the patient;
- Failure to exercise appropriate supervision over persons who are authorized to practice only under the supervision of the physician;
- Ordering of excessive tests, treatment, or use of treatment not warranted by the condition of the patient;
- Failing to wear an identifying badge, which shall be conspicuously displayed and legible, indicating the practitioner’s name and professional title while practicing as an employee offering health services to the public;
- Failure to use scientifically accepted barrier precautions and infection control practices as established by the Department of Health pursuant to section 230a of the public health law.
FACULTY ADVISORS
Each resident will be assigned a faculty advisor. The role of the advisor is to facilitate the resident’s progress through the residency. The resident is encouraged to utilize his or her faculty advisor with all aspects of resident life. Faculty advisors should be a source of feedback and inspiration for the residents. The faculty advisor may be particularly helpful in assisting the resident to achieve set academic goals. It is required that the faculty member and the advisee meet at least every three months to review the resident’s progress. The faculty advisor is also required to review the monthly patient follow-ups. Residents may ask their advisors to be present during their bi-annual evaluation with the residency director and during any remediation discussions with the residency directors.
It is the resident’s responsibility to approach his/her advisor. If there are problems scheduling a meeting with your advisor or you would like to change your advisor for any reason, please let the Residency Directors know.
However, the role of the advisor shall not be limited to mandatory meetings but shall be proactive and visible in the resident’s academic development.
This can be accomplished in a variety of ways and should consist of, but not be limited to, some of the following:
- Literature review
- Reading assignments
- Meetings with oral board type scenarios
- Case review
- Review of advisee’s follow-up sheets
- Round table discussions
- Question & answer settings
- Review of multiple choice questions
- Review of ethical and administrative issues
- Review of resident’s procedural skills and help in achieving excellence
- Review of the resident’s ethical and professional growth and guidance towards excellence
- Mentoring during times of personal duress or stress
- Resolution of conflicts with the department or other staff
NOTE: A Resident Evaluation Form (located outside Ms. Lane’s office) may be used as a guideline for resident-advisor meetings to address certain issues and to document regular meetings. This form must be given to the residency coordinator to be placed in the resident’s file.
Please inform the Residency Directors (specifically, Dr. Quinn) if there are any problems with meeting with your advisor or if you wish to be assigned to a different advisor for any reason.
SICK CALL POLICY
The Department of Emergency Medicine has set up a sick call beeper system to cover the ED when residents are ill or unable to work scheduled shifts. During the PGY-2 and PGY-3 years residents will be assigned two separate two-week blocks of sick call.
Historically, these rotations have been during non-ICU and non-ED rotations, such as ENT, Ultrasound, Toxicology, and Research. While on sick call, the resident might be called to cover any sick EM resident scheduled for the UHB & KCH adult or pediatrics EDs.
Typically, PGY-2 residents cover junior residents and PGY-3 residents cover senior residents. However, at the discretion of the EM Chief or residency directors, any sick call resident may be activated for any sick resident irrespective of year or parent department.
The sick call resident will carry the sick call beeper for the entire time on sick call and is expected to be available and free from the influence of alcohol or other substances at all times during their call period, including weekends and nights. The resident must also stay within beeper range of the hospital. If you need to leave the NYC area then arrange coverage from a peer.
The resident who is receiving the pager at the time of turn over is responsible for obtaining the pager. Not having been given the pager is not an excuse to miss a call. Any resident who is unavailable during their sick call will be held accountable for the missed clinical time.
The sick call beepers are usually used when another EM resident calls in sick, the ED is busy, and extra help is required to ensure adequate patient care. Do not abuse the Sick Call System. It is not to be used for recreational or personal needs.
The only people who are authorized to activate the sick call resident are the Chief-on-call or one of the Residency Directors. If the sick call resident is called in by another person, the called resident is to immediately refer the matter to the Chief Resident on call or one of the residency directors.
The following is the procedure for an ill resident to activate the sick call system:
PLEASE NOTE:
NOT ADHERING TO THESE PROCEDURES HAS CAUSED MAJOR PROBLEMS IN THE PAST. THEREFORE, STRICT ADHERENCE IS MANDATORY AND WILL BE ENFORCED.
Sick Call Procedure: KCH and UHB ED
- This procedure has to be followed for all rotations- yes, every single rotation.
- For clinical rotations, check to see if there is anyone who can switch with you. Contact that person. You must call the Chief-on-call either way. If you can find coverage for yourself, call the chief-on-call and tell the chief who will be covering your shift. If not, you need to call the chief-on-call and tell them that you will require sick call coverage.
- You must call the Residency Director on call (pager no.: 1-917-219-0650,
and the chief on call (1-917-761-1405.) If you cannot reach a director via pager, then feel free to call the directors cell phone (see below) and leave a message on their cell phone voicemail. NOT CALLING IS UNACCEPTABLE UNDER ANY CIRCUMSTANCE UNLESS YOU ARE INTUBATED.
- You must leave a message with the Residency Coordinator (718-245-3318)
- A Residency Director and/or the Chief-on-call will decide IF the sick call resident will be called after evaluating present coverage and the state of the clinical area involved. We only use sick call when absolutely necessary.
- **Only the Chief-on-call or one of the Residency Directors can activate the sick call coverage system.**
- If you need to call out for reasons not related to your personal illness or death in the family, please attempt to find your own coverage. If you cannot find your own coverage, then contact the Chief and director as is the current policy. You must pay back the sick call person any shift, which was covered for reasons not related to personal illness/family death.
- If you are the pre-attending at KCH, the pretending needs to try to find their own coverage. However, if a pretending calls out, we will float a PGY 4 from a different location. The PGY 3 on sick call will then fill the hole where the PGY 4 vacated. The PGY 4 who called out will then have to get one more pod A shift in the next block and the PGY 3 who covered will get one more shift in the location that they were pulled from. Worst case is we will not have a pretending that shift but this is a last resort.
Sick Call Procedure: Off-service and Affiliate EDs
Same as above, in addition:
- You must notify the clinical site director for ED rotations and the Chief residents for off-service rotations.
- Residents will adhere to established sick call policies at these sites.
- Any difficulties with sick call policies should be referred to the Residency Directors.
- You must call the Residency Director on call (pager 917-219-0650).
- You must leave a message with the Residency Coordinator (718-245-3318)
Sick Call Procedure Conference Days
- You must make 70% of conference days. There is no negotiation on this point. If you are sick, don’t come in. However, if you miss more than 30% of all conference days for ANY reason, then you cannot graduate the program until this is rectified.
Cell Phone numbers
Smith (347) 768-2933
Khadpe (610) 657-9221
Rios 917-693-4429
Silverberg 917-822-4510
Quinn 718-938-4841
Pager numbers
Chief on call pager 917-761-1405
RD on call pager 917-219-0650
Phone numbers
Residency Coordinator 718-245-3318
UHB Adult ED 718-270-4580
UHB Peds ED 718-270-8267
UHB Fast Track 718-270-8289
KCH Adult ED 718-245-4616
KCH Peds ED 718-245-3638
KCH Critical Care ED 718-245-4603
KCH Fast Track 718-245-4610
LICH Adult ED 718-780-1961
ED CONFERENCE ATTENDANCE POLICY
Conference attendance is mandatory. All residents must attend conference. Those excused include:
- Residents on vacation
- Overnight Shift: These residents must attend one hour of conference, after which they are excused, and will receive full credit for conference attendance.
- Late shift on Tuesday/Wednesday: These residents are allowed to be late one hour to conference, i.e. arrival at 9am. Please refer to AGME/NY State guidelines.
- Sick Day: must call Education Chief (Cassandra Bradby) and Residency Director on Call to explain why you are not attending conference. A record will be kept to tally how many sick call requests from conference you have taken in the year.
- Off Service Rotations/Electives: For all off-service rotations at KCHC, excluding the ICU and Medicine rotations, the resident is expected to attend conference for at least 2 hours for full credit – this is a required part of education and should be excused by the off-service team.
For all unexcused absences from conference, you will receive an extra shift. If you do not call out to the Educational Chief and DOC for an appropriately excused absence from conference, you will incur an extra clinical shift. If you come more than 5 minutes late, it will be recorded. If you are late 3 times, you will incur an extra clinical shift.
RRC requires that every EM resident must be present for 70% of the Wednesday conferences during their entire residency training (35% for EM/IM residents). The attendance statistics will be posted on the conference room door approximately every quarter. You must be there for the full 4 hours to get credit for the day if you are not scheduled to work that day (late Wed shift) or the night before (late Tues shift). If you leave early or come late outside of the current handbook policy on Wednesday conference attendance, you will not get credit for that conference day.
It is your responsibility to keep track of your conference attendance and know how close you are to that 70% level. This number can be reviewed with a residency director at your 6-month evaluation meeting or you can make an appointment with a director to discuss this at any time. It is also posted each quarter.
If by some terrible chance of “luck”, graduating residents are below your required 70% (35%), they will have to attend conference during their elective or during July to make the minimum requirement in order to graduate the program. The 70% (or 35% for EM/IMs) RRC conference attendance requirement is not negotiable and you cannot graduate from ANY EM residency without fulfilling it.
Missed Requirements Policy
Even though residency is an extension of your education to becoming a competent Emergency Medicine physician, it is also a job. As with any job, there are consequences for not fulfilling job expectations. This policy delineates the consequences for not following the rules and regulations set forth by the conference and extra-conference faculty liaisons. Please consult the sections of the handbook for the specific requirements for each division and clinicalmonster.com for all schedules (i.e. simulation, board review, lecture preparation, skills labs).
Whenever a resident fails to meet a specific job requirement, he or she accrues 4 to 8 hours of clinical time based on the severity of the infraction judged by the Program Director. For every 8 hours accrued, the resident will be assigned to work an 8-hour shift by the KCH scheduling chief resident. The residency leadership understands that unforeseen circumstances can occur, which accounts for only 4 clinical hours to be accrued for the first occurrence of minor infractions. This policy applies to but is not limited to the following:
- Missing a required simulation session
- Missing a required board review session
- Missing a required skills labs
- Failure to prepare for board review sessions as described in the handbook
- Failure to submit lectures for review by the required deadline
- Failure to come in for a shift
- A pattern of chronic lateness to shifts
The residency leadership reserves the right to review each case, depending on the circumstances of the situation.
WORK ATTIRE POLICY
We all realize that the hospital is not the cleanest place in the world. Therefore, wearing fancy clothes can become taxing on the wallet when dry cleaning bills and replacements for destroyed garments start to stack up. However, as dirty as the ED may be, we still need to look professional. While we do not want to enforce a strict dress code, we would like to set a standard.
When working clinically at Kings County, scrubs are acceptable although we encourage professional casual dress when working in the non-procedure oriented areas such as Pod A. Jeans are never acceptable and neither is any shirt that does not cover the entire abdomen. When working in UHB, men should try to wear khaki pants or slacks and a button down shirt while women can wear a similar ensemble or something equally as professional. Additionally, we should also think about what we wear to our academic Wednesday conferences. This is especially true when an outside speaker is going to be present. When giving a lecture, looking the part is very important. If you are giving a lecture, you should have professional attire or business casual. This means:
1. No scrubs when giving a lecture. If you are working at 12 noon or worked the overnight, you can change into your scrubs before or after your lecture
2. No jeans, t-shirts or sweatshirts when giving a lecture
3. The lecturer should wear business casual, which means an ironed shirt, pants, blouse, dress etc.
If you have questions, you can check out the link below for some additional examples.
http://www.career.vt.edu/Jobsearc/BusCasual.htm
You put a great deal of effort into your presentations. Look the part and complete the package. If you have any questions, please feel free to contact your faculty advisor or any one of the residency directors with additional questions.
"The difference between greatness and mediocrity is in the detail."
MOONLIGHTING
Moonlighting during residency is a controversial topic in Emergency Medicine. A number of residents moonlight to make some extra money and for the added clinical experience of practicing in a different environment. Supporters of moonlighting feel it can be an important transition towards solo practice. The department’s stand on moonlighting is neutral; however, residents who moonlight will have to get approval from the Program Director. This approval is contingent on satisfactory clinical and academic performance (including the in-training exam). The Program Director has final say on moonlighting privileges.
Moonlighting at other institutions is only allowed in the graduating year and CAN NOT BE IN A SINGLE COVERAGE ED. There must be a board-eligible EM attending working with you, even if you are functioning as the attending. This is to protect you and the integrity of the specialty.
There will occasionally be opportunities to “moonlight” at KCH, UHB, or LICH. These shifts are paid, cannot be in conflict with your other residency responsibilities, and are under the supervision of EM faculty. You function as a resident during these shifts, not as an attending. These shifts are allowed at the discretion of and with the agreement of the residency directors and the medical directors. This approval also is contingent on satisfactory clinical and academic performance (including in-training exam).
All moonlighting schedules have to be reviewed with the program directors prior to the beginning of the month. The purpose of this is to ensure moonlighting does not compromise any resident’s departmental duties as well as educational obligations. Moonlighting may also not interfere with ACGME or the New York State DOH 405 regulations. All internal and external moonlighting counts towards the duty hours limits.
Please note, that failure to adhere to this policy will result in loss of moonlighting privileges and/or other adverse actions. Moonlighting without the permission of the Program Director is a serious act of misconduct.
POLICY ON CHIEF RESIDENT SELECTION
Being a chief resident is a challenging and rewarding experience. Chiefs will gain a tremendous amount of supervisory and administrative experience during that year. Chief residents in the program are graduating year residents and are elected for service by the Program Director, the faculty, and the residents (all have equal vote).
Our chief resident selection is very close to a completely democratic process. However, the Program Director reserves the right to make final decisions and alterations in this selection process that he/she feels is in the interest of the program and the department.
The normal procedure for chief selection is as follows:
- Residents of the appropriate year will have an opportunity to add or remove their name for consideration for chief resident.
- This list will be approved by the Program Director in consultation with the residency and departmental leadership.
- Residents that have been on Academic Probation for clinical, academic, or professional reasons are not eligible for chief candidacy.
- The Program Director can remove candidates from the list if he/she feels that that candidate cannot serve effectively in the chief resident role.
- The final list becomes a ballot and is voted on by the entire department with 1 vote for each physician. The residency coordinator also has 1 vote.
Chief residents are selected from both programs. The combined resident with the most votes will become a chief. Additionally, the four categorical residents with the most votes will become chiefs. Only 1 EM/IM residents can be selected as chief. The chief of the EM/IM program will always be an EM/IM resident. This process can be altered by the program director if he/she feels it is in the best interest of the program.
Chief candidate qualifications:
- Model resident
- History of strong contribution to the residency and department
- Academically solid
- Superior leadership skills
- Strong interpersonal and communication skills
- Has not been on probation or formal remediation during the program
- Holds a valid NYS medical license
ON CALL ROOMS AT KCHC
There are two on-call rooms available to KCH EM residents. The rooms are located in the T-building on the 8th floor and are available on a per day basis for the residents. The rooms are for all EM residents to use and squatters will be asked to move out their belongings if they prevent other EM residents from access to the rooms. Room keys are available from the residency coordinator.
If keys are needed for the weekend, please contact the residency coordinator in advance.
EMPLOYEE HEALTH SERVICE (EHS)
In addition to your provided health care coverage each affiliate institution maintains an employee health service center. The health service center is responsible for a number of resident related issues. Each resident must obtain and maintain health clearance from the institution responsible for their salary. This usually entails an initial health screening exam and verification of PPD status and immunizations. Periodically employee health services may request repeat PPD testing and other occupational health care related training (e.g. respiratory isolation mask fitting). The other time employee health service may be utilized is with respect to illness or injury at work. One important injury that EHS is responsible for is follow up on all occupational exposure to blood borne pathogens. All needle sticks at Kings County irrespective of resident pay source are referred to KCH EHS after initial care is provided in the Treatment Room. KCH EHS is to forward all needle stick paperwork and laboratory results to the residents’ payroll institution after the initial follow up visit.
Employees Health Contact Numbers:
Kings County (718) 245-3536
UHB (718) 270-1995
NEEDLESTICK/BODY FLUID EXPOSURE PROTOCOL
Occupational exposure to infectious disease is an obvious concern at Kings County and its prevention is a priority of the department. Recently, the Centers for Disease Control has issued a recommendation concerning occupational exposure to infectious bodily fluid and the possible use antiviral medications. Please review this material and be familiar with what to do if you or a colleague suffers a body fluid exposure or needle stick. Please remember to check your Hepatitis antibody status and take appropriate steps when indicated.
All employees, residents, students, or visitors to Kings County Hospital who sustain an exposure are to be seen in the Emergency Department (24 hours a day). The needle stick packet is available at all time in the ED and has to be completed by the attending physician or an ED resident. The recommendations for antiviral medications are enclosed in the needle stick packet and if antiviral therapy is initiated the first dose will be distributed from the supply in the Treatment room.
Dr. Jacques, the ID specialist, should also be paged (917-486-2623, or office x 3716) to follow up on all needle stick prophylaxis.
At discharge the exposed patient should be given a prescription for a five-day supply. The prescription should be filled without charge in the pharmacy for all residents. Needle stick packets should be filled out completely and given to the ED Administrator on duty. Also exposed patients and agreeing source patients should have “needle stick” bloods drawn at the time of injury. The computer has a predetermined panel that may be selected that includes all needed blood test except HIV testing.
Both the source patients and exposed health care workers can be counseled and consented for HIV testing using the consent forms in the needle stick packet.
Please follow the instructions affixed to the packet for proper processing.
All employees and residents are to follow up in employee health services the following working day.
Any questions, please contact Dr. Rinnert at: 718-24594790 (office) or 917-761-1142 (beeper) or cell (646) 319-7077
Institutional Policy ON DISCRIMINATION & SEXUAL HARASSMENT
Discrimination: SUNY Downstate does not discriminate on the basis of race, sex, color, chosen gender, religion, age, national origin, disability, marital status, status as a disabled veteran or veteran of the Vietnam era, or sexual orientation in the recruitment and treatment of students and residents.
Sexual Harassment: In keeping with the University’s efforts to establish an environment in which the dignity and worth of all members of the institutional community are respected, sexual harassment of students and employees at Downstate is unacceptable conduct and will not be tolerated.
Sexual harassment may involve the behavior of a person of either sex against a person of the opposite or same sex, when that behavior falls within the following definition: Sexual harassment of employees, residents, and students at Downstate is defined as any unwelcome sexual advances, requests for sexual favors, or other verbal or physical conduct of a sexual nature, when: (a) Submission to such conduct is made either explicitly or implicitly a terms or condition of an individual’s employment or status as a student; (b) Submission to or rejection of such conduct is used as the basis for decisions affecting the employment or academic status of that individual; (c) Such conduct has the purpose or effect of unreasonable interfering with an individual’s work performance or educational experience, or creates an intimidating, hostile or offensive work or educational environment. A hostile environment is created by, but not limited to, discriminatory intimidation, ridicule or insult. It need not result in an economic loss to the affected person.
Complaint Procedures: Persons who feel that they have been subject to prohibited discrimination or who have been sexually harassed under the above definition and wish further information, or assistance in filing a complaint, should contact the Affirmative Action Officer at (718) 270-1738, Room #5-82 C, Basic Science Building. Any resident that feels they have a complaint can also bring that issue to the Program Directors or the Departmental Chairman.
FAMILY MEDICAL LEAVE ACT
Effective February 5, 1994, all employees are eligible to request unpaid leave charged to leave credits under certain circumstances, for a period of up to 12 work weeks in a 12-month period due to: 1) the birth of a child or the placement of a child for adoption or foster care; 2) the employee’s need to care for a family member (child, spouse, or parent) with a serious health condition; or 3) the employee’s own serious health condition which makes the employee unable to do his or her job. Under certain conditions, this leave may be taken on an intermittent basis.
Employees are also entitled to continuation of health and certain other insurance, provided the employee pays his or her share of the premium during this period of leave. Upon return from FMLA leave, most employees must be restored to their original or equivalent positions with equivalent pay, benefits, and other employment terms. FMLA makes it unlawful for any employer to 1) interfere with, restrain, or deny the exercise of any right provided under FMLA, or 2) discharge or discriminate against any person for opposing any practice made unlawful by FMLA or for involvement in any proceeding under or relating to FMLA. The U.S. Department of Labor is authorized to investigate and resolve complaints of violations. An eligible employee may bring a civil action against an employer for violations. For additional information, contact SUNY Labor Relations at x3019.
Please note, that since residency is a structured educational process requiring a minimum number of months of training for Board eligibility you may take FMLA but you will need to make up the months. In other words you may end your residency at a later date.
Currently, you can only miss 6 weeks in any give academic year for any reason including vacation. This leave can NOT be transferred from year to year. Any missed time over this limit must be made up.
THE IMPAIRED PHYSICIAN
Physician impairment through alcohol and drugs is a widely recognized problem. Residents in high acuity, high stress environments are particularly prone to fall victim to alcohol and drugs. The University has outlined guidelines in its SUNY Resident Handbook on how to deal with impairment. Please refer to the appropriate pages of the SUNY Resident Handbook.
If you should notice any impairment in yourself or your peers and need help in dealing with it, please contact your faculty advisor, your Residency Directors, or your Chief Residents.
Since we are in a highly visible field of service AOB (=Alcohol on Breath) is viewed as absolute unprofessional behavior and an early sign of a possible underlying problem.
Physicians appearing to having a drug or alcohol problem will be referred to the NYS Committee for Physician’s Health.
Emergency/Disaster Preparedness 2013-2014
Preparation for emergencies is a well-developed sub department at SUNY Downstate and Kings County Hospital Medical Center. The New York Institute All Hazard Preparedness has been a funded part of the Emergency Medicine Department since 2002. We work with other departments at SUNY, nationally and internationally on various research projects including but not limited to, Community Wide disaster drills, creating policies for vulnerable populations during a disaster, Ethical issues in a Disaster, and Critical Care throughput during a mass causality event. We have contingency plans for ensuring that the Medical Centers would continue to operate in times of disasters.
The hospital’s plans are updated and maintained by the Emergency Preparedness Committees of University Hospital, Long Island College Hospital and Kings County Hospital they can be found on the web at:
http://www.downstate.edu/emergency_medicine/disasterplans.html
The Emergency Management Plans are “All Hazard Plans” as required by Governmental and Joint Commission Standards. The Plans also address how the Medical Centers will respond to Nuclear/Radiologic, Biologic and Chemical and Mass casualty incidents. The Medical Centers have committed significant resources towards the development of a Hazardous Material (HAZMAT) Decontamination System, which includes representatives from the Emergency Department, University and Hospital Police, facilities and Environmental Services. All incoming interns are trained in HAZMAT protocols. There is an ongoing effort to enroll and train the nursing staff as well. This team is trained and certified in emergency decontamination procedures. In addition, we are committed to awareness level training in HAZMAT for all employees.
As part of our emergency preparedness efforts, both institutions conduct at least two drills per year. All residents participate in these drills. Through these drills we continue our research in disaster response systems.
The SUNY/KCHC Fellowship in Emergency Preparedness started in July 2005. The fellowship is a 1 or 2 year program.
Goals for the future: At all three hospitals we are committed to large ongoing educational programs for all departments of the hospital. We work with each department on their disaster plan and insure that it integrates well with the hospital-wide plan. We have enacted The Hospital Incident Command System (HECS) and on-going education continues. At the same time EM residents are actively involved in the Disaster Committees. They participate in local, state, national and international conferences in emergency medicine representing the disaster committees of the hospitals. Research continues on how best to prepare for disaster in hospitals that share resources. We will be continuing to forge a community response in Brooklyn with additional drills and trainings. Current resident projects include: surge capacity research, equipment management, hospital disaster training and education, and participation in the management of the Medical Student Support Team to name a few. We participate in INDUS-EM collaboration with All India Medical Institute, Medical College of Boroda and the University of South Florida.
Terrorism continues to be a threat in the United States and large accidents or natural disasters occur daily. These events can drain the resources of even the most prepared hospital. As members of the Medical Center community, we all have important roles in our disaster plan. It is important that you know your role in the plan as well as our department’s responsibility in times of an emergency. This will help ensure that we will always be able to provide the best care for our patients. A basic outline of the steps to take if a disaster is declared is attached for review. Please read this document and review your specific Emergency Management Plan.
Thank you.
Bonnie Arquilla, DO
Associate Professor Clinical Emergency Medicine
Director Emergency Preparedness
SUNY Downstate Medical Center
Kings County Hospital Medical Center
Long Island College Hospital
WHAT TO DO IF A DISASTER IS DECLARED
· Your department has a plan. Do not leave your regular post/job unless you are instructed to do so by your departmental plan or supervisory personnel.
· Do not under any circumstances speak to news media. Refer them to the Office of Institutional Advancement of UHB or Media Relations of KCHC.
· No visitors are allowed in the hospital during a disaster. Send all visitors to the Family Reception Area in the Cafeteria of UHB or T-Building of KCHC.
· Activation of the plan occurs in phases:
- Potential: Limited departmental notification – no staff changes.
- Actual: Limited or complete notification –possible staff changes.
· The Hospital plan is an All Hazard Plan: Any disaster inside the hospital or on campus that endangers patients or staff and creates a possible need for evacuation or relocation.
· Anyone who learns of an occurrence that might constitute a disaster should attempt to obtain the following information and contact the Administrator on Duty immediately: In the emergency department the CCT attending or UHB Main ER attending can declare a disaster for a Mass Casualty, if unable to contact the AOD.
- What was the occurrence?
- What is the location of the occurrence?
- How many casualties are estimated?
- What are the types of injuries?
- How many people were injured?
· 4-4-4-4 Bells or CODE D means an Actual Disaster is in progress in UHB.
· 2-2-2-2 Bells or CODE Yellow means an Actual Disaster is in progress in KCHC.
· The Emergency Operations Center coordinates all resources during a declared disaster.
· The Disaster Cabinet and Mass Casualty Incident (MCI) Packets are in the Emergency Department Ambulance Entrance.
· All patients/victims will enter through the designated areas for primary triage. Direct all victims to that location to assure that they are evaluated and treated in order of need, given the best and fastest care possible and prevent hospital contamination.
· Where will overflow patients at KCHC be evaluated and treated?
D Building Lobby Minor Medical & Minor Trauma
Peds E building Peds Medical and Peds Minor
R Building Behavioral Health
· Where will overflow patients at UHB be evaluated and treated?
Adult Emergency Department Major Casualty
Pediatric Emergency Department Peds Major Injury
Suite A Minor Medical
Suite B (Waiting area) Minor Trauma
Suite D Peds/Medical Minor Trauma
Suite I Behavioral Health
Suite J Eye Trauma
· After the evaluation and treatment of minor patients is complete, they must go the Family Reception Area to complete the proper paperwork arrange for follow up and be discharged. The Family Reception Area is in the Cafeteria at UHB. It is in the T-Building 1st floor at KCHC.
· The Nursing Staff Resource Pool is in the Nursing Office.
· De-escalation and Stand Down: At UHB the All Clear signal is 1-1-1-1 Bells. At KCHC the All Clear signal is a verbal overhead announcement, “This is an all clear.”
· Debrief: Report helpful comments recommended changes to your Department Head.
STUDENT EDUCATION
As you learned during the SUNY-Brooklyn orientation, you will be part of a resident development program. The program is designed to help you gain the skills, which are necessary for you to excel in emergency medicine in a teaching forum. Our University system is an academic institution, which is dedicated toward fulfilling the mission of patient care, education and research. Patient care will come with experience, research will go on all around you, but education is something we all must actively pursue.
It will be a rare clinical moment when you find yourself entirely without a single student. Whether they are physician assistants, nursing, military or medical students, they depend on you for their education. You have the unique opportunity to impact the career development of your colleagues and future health care providers of our nation. We expect you to take this responsibility seriously. Teaching students is part of our job. It’s not a burden; it’s a privilege.
We all “carve out” a piece of time during our busy day to teach. Hopefully, you will become proficient at it and even enjoy teaching. Teaching is as rewarding as a handshake from a patient or a smile from a child. It is one of the reasons why we put on that stethoscope each day.
Look out for the students when they are in the clinical area and get them involved in good cases. They should be able to see most cases by themselves, however you will need to assess their learner level and supervise them accordingly. I.e. if you see them getting hung up on a particularly difficult case----bail them out.
Residents are asked to guide students through the SUNY Downstate/Kings County system (i.e., how to send labs, where supplies are, how to get medications, etc.). Senior residents and attendings will be asked to help with the didactic portion of the student rotation. Responsibilities during the “Teaching Resident” direct supervision of students in the clinical area. Many residents also participate in medical student education activities such as patient simulation cases and interactive case-centered student lecture. Please contact the student education directors if you are interested.
General Guidelines in clinical area:
- Before/after clinical rounds, the senior resident is charged with identifying and distributing the students appropriately between EM residents and faculty. The attending and senior resident should communicate with each on how best to do this depending on the physician coverage and # of patient in the area.
- In general, students should be paired with EM residents, preferable PGY2, 3, 4, 5 but an EM PGY1 is ok if no other EM resident available. Specifically, MS4 Elective students, who are seeking LORs (letters of recommendations), should be paired with the attending (1:1 or 1:2). Please note, in some cases, the student may have changed their shift to work with a particular attending on shift. If for any reason, there are too many elective students for one attending, they may work with the senior resident. Clerkship students (MS3/MS4-on their first EM rotation) should be paired with residents.
- Residents are primarily responsible for the patients they supervise with the students. In the case of senior elective students who are working with the faculty, senior residents may hear student case presentations, and then help them organize the case for formal presentation to the attendings.
- Since every clinical area in our dept. is variable, it is good to give your student guidelines of your expectations: pick up patients vs. assign patients, prepare H&P and A/P with differential diagnosis, follow through and taking ownership of patients, write-ups.
- ALL students are required to write-up their patients. Its part of their education to learn appropriate documentation. Review write-ups as time allows in the clinical area.
- Return an evaluation for every student you work with within 48 hours or less. Either paper in the metal drop boxes in the clinical areas or electronically on New Innovations. (If you receive a New Innovations evaluation—just write “done on paper”). The dual system is necessary until the school converts to web-based evaluations completely
- Sign-off on all required logs and attendance sheets with STAMP.
Student requirements:
- Write up every patient. Resident should review as many as possible. Clerkship has a minimum required 2 write-ups for review and feedback by supervising physician. Its part of their education to learn appropriate documentation.
- Case-log of chief complaints. This is a minimum requirement for students. Please help students identify patients to complete this log.
- Basic procedures log and attendance sheet.
- Provide an evaluation for every shift worked with faculty/resident.
- Mandatory lectures every Thursday mornings. Scheduled simulation sessions on Tuesday mornings. Elective students have Thursday afternoon additional sim and skills labs and presentations. Clerkship has an exam on last Friday of rotation.
As of August 2013, a new medical school curriculum will be implemented, the Integrated Pathway Curriculum (IPC). The new curriculum will teach and assess the knowledge, skills and attitudes that fall under the six Domains of Competence, modeled after the ACGME. In the IPC the required EM rotation will expand to a required four-week advance student rotation in the 4th year, which will be in effect 2015. Until this date, we will be transitioning away from the required two-week clerkship for third year students.
Our department offers the following student rotations in the upcoming academic year:
1st Year Students:
- Doctoring experience: each MS 1 will spend one evening in the ED, preceded by a short introductory lecture and followed up with an experience summary
- Emergency Medicine (observational) elective: a selected number of first year students spend one evening a week for 6 weeks shadowing physicians in the ED.
- EM Ultrasound curriculum incorporated into new curriculum
- Patient Simulator curriculum incorporated into new curriculum.
2nd Year Students:
- Emergency Medicine (observational) elective: a selected number of second year students spend one evening a week for 6 weeks shadowing physicians in the ED
3rd Year EM Core Selective
- 2-week Selective intended for career exploration during the clinical years.
- Exposure to the clinical responsibilities of the ER as well as the various sub-specialty fields. Students will work at least one shift in the following clinical areas: critical care/trauma, adult and pediatric areas with select faculty.
Mandatory EM Clerkship:
- As of 2000 every medical student has a mandatory 2-week Clerkship rotation in the ED (primarily MS4’s, but select exemption given to MS3’s interested in EM). Students on this rotation should present primarily to residents, but depending on ED staffing they may also present to the attending.
- As of 2015, the rotation will be 4-weeks and only for MS4’s.
4th Year Students:
- Four week EM elective: these students are interested in EM. They may present primarily to the faculty, as they are interested in LORs. However, depending on ED staffing, they may occasionally have to work with a senior resident.
- Two week advanced EM elective (CCT)
- Peds EM elective (2 or 4 weeks)
- Advanced Preceptorship elective - “Follow an Attending”
- EM Ultrasound elective
- EM Brooklyn VA elective
Other departmental medical student involvement:
- First year anatomy lab clinical correlation
- Second year phlebotomy labs
- Participation in the first year mentoring program
- Participation in the problem based learning program
- Participation in the Preparation for Clinical Medicine Course - First Year
- Participation in Foundation years clinical diagnosis, physical exam courses (lectures, small group facilitators)
- Emergency Medicine lectures for the Physician Assistant Program
- Serve as mentors for the Sophie Davis Educational Program (Advanced placement Minority Student Program)
- Frequent lectures to the Emergency Medicine Club
- Pre–med college student observational clerkship
- First/Second year suture lab
- Second year physical examination course
ONLINE RESOURCES / CIS / INTERNET / EMAIL / TECHNOLOGY
SUNY Downstate / Kings County Emergency Medicine Website
The official department website is located at downstate.edu/emergency_medicine

Additionally, the Education division in coordination with the founder, current EM/IM resident Michael Ritchie, maintains an online repository of residency resources on Clinicalmonster.com

The site maintains links to all clinical and academic schedules, institution specific clinical resources, New Innovations, Evaluations Manager, Wednesday conference information, asynchronous learning activities, the educational residency weblog, and many other useful residency resources.
A copy of the Residency Handbook is available online on Clinicalmonster.
Many of the online resources are password protected. The username/password is always “suny”.
The Downstate Library website serves as a portal to a host of medical journals (Serials) and a variety of evidence based-medicine resources (EBM Resources).

For access, most Downstate library resources will prompt you for a username and password. Your username is your full name as printed on your Downstate ID and your password being the 16-digit number immediately below your name (not the Lib#).
The ClinicalMonster site also contains a dedicated online resources section with links to various free educational resources in addition to the Downstate library.
Each resident participates in a training session for the clinical information systems used at Kings County Hospital and SUNY Downstate. The product used at Kings County is Quadramed. The product used at SUNY Downstate is the electronic T-System.
Internet Access at Kings County Hospital
Every resident is authorized to have Internet access at Kings County Hospital. You will receive a username and password, which will be prompted when you attempt to access most sites outside of the Kings County Intranet. Internet access through Kings County is limited without a username and password. Restrict your browsing to clinically relevant domains. Completely close your web browser windows when you are finished, as your Internet activity is monitored. Without a password, you should still be able to access your Downstate, Yahoo, Hotmail, and Gmail e-mail accounts and most clinically relevant sites.
Internet Access at SUNY Downstate Hospital
Every resident is authorized to have Internet access at SUNY Downstate Hospital. There is no username or password required to get online, however some sites are blocked by the firewall. Again, please restrict your browsing to clinically relevant domains.
All residents need to maintain at least one email account for all residency related communications and keep Ms. Lane up to date with that address. This email address should be used for membership to the SUNY EM Yahoo! Group (a mailing list) and you should check it on a regular basis for departmental communications. Additionally when sending protected health information (PHI) via email, you must use a dedicated KCH or Downstate email address for each institution’s respective PHI.
In addition to the computers in the clinical areas, there are computers in the resident’s lounge with the Microsoft Office suite and Internet access.
Smartphone/Tablet Applications
Faculty and residents use a variety of medical apps when working in the department. Feel free to ask individuals about their thoughts on apps that are most useful.
Website/Technology Development
We are looking for help in further development of our website and electronic resources. Any resident with interest in these areas is encouraged to join the Department’s Technology Committee. Contact Dr. Khadpe for more information.
There is a slide maker and scanner in Dr. Sinert’s office that residents may use for presentation preparation. A digital camera for departmental photos is kept in the program director’s office.
MONTHLY SCHEDULES
KCH ED/Peds ED:
The Scheduling Chief Resident is responsible for the making and distribution of the monthly KCH ED schedule. He/she is the most important person with respect to the intricacies of the daily schedule and is the first person to approach with scheduling questions and requests. The Scheduling Chief Resident must approve all schedule changes. Late requests will not be honored. Requests are a consideration, NOT guarantees. Exceptions are to be discussed in advance with residency directors and chief resident.
Considerations for schedule requests:
- All requests for health and educational leave will be granted first.
- If going away, request travel days as well as days away off.
- There is a limit of three separate requests per month. They will be honored on a priority basis, so choose your top choice carefully. There will be a maximum of 3 days off in a row depending on coverage. If any request for greater than 3 days is received it will be disregarded unless it has been approved by the residency directors. The only exceptions are academic meetings and conferences.
- Note that the schedule historically goes through revisions in the first weeks of the month, so check it frequently. Once revised, the new copy will be posted on the bulletin boards in the ED Administrative area and one in the clinical area.
- Please check the schedule, even if you requested certain days off. Requests are not guaranteed, but every effort will be made to honor them.
Nights
All residents will work 40-50% night shifts in the KCH ED and 50-60% nights in the Peds ED. Every effort will be made to group the night shifts together.
Weekends
All attempts will be made to give residents at least one Saturday and one Sunday off per clinical rotation – scheduling permitting.
Distribution of shifts
- The ratio of shifts in each clinical area will be grossly equal across PGY level. Coverage may dictate that this balance varies somewhat.
- PGY 3 and PGY 4 residents will do KCH Pediatric and Adult shifts during the same month. Junior residents will have month long rotations in Pediatric EM at KCH.
Special Shifts and Wednesday Conference
Junior residents (PGY 1 and PGY 2) will have the majority of Tuesday PM shifts off to enable their attendance at conference. Residents have to report to the clinical area immediately after conference. Senior residents may be scheduled for one Tuesday overnight, one Wednesday AM and/or Wednesday PM shifts as coverage dictates. The scheduling chief resident may have the residents scheduled for shortened shifts after conference as coverage dictates. Senior shifts scheduled 11AM – 7PM and Junior shifts scheduled 7AM-7PM begin at 12 Noon.
The following are the updated requirements for conference attendance that take into account resident work hours and current ACGME and NY State guidelines. If you have any questions as to whether or not you need to attend conference please contact me as soon as possible.
KCH |
|
|
Tuesday Shift |
Wednesday Shift |
Attend Conference |
Off |
3PM-11PM |
7AM-Noon |
Off |
11PM-7AM |
7AM-11AM |
Off |
7PM-7AM |
Off |
7AM-3PM |
3PM-11PM |
7AM-Noon |
7AM-3PM |
11PM-7AM |
7AM-Noon |
7AM-7PM |
7AM-7PM |
7AM-Noon |
7AM-7PM |
7PM-7AM |
Off |
9AM-9PM |
Off |
7AM-Noon |
11AM-11PM |
Off |
9AM-Noon |
11AM-11PM |
11AM-11PM |
9AM-Noon |
11AM-11PM |
7PM-7AM |
Off |
3PM-11PM |
Off |
9AM-Noon |
3PM-11PM |
3PM-11PM |
10AM-Noon |
3PM-11PM |
11PM-7AM |
9AM-Noon |
7PM-7AM |
Off |
7AM-9AM |
7PM-7AM |
7PM-7AM |
Off |
11PM-7AM |
11PM-7AM |
7AM-9AM |
11PM-7AM |
Off |
7AM-9AM |
|
|
|
UHB |
|
|
Tuesday Shift |
Wednesday Shift |
Attend Conference |
7AM-5PM |
Off |
7AM-Noon |
7AM-5PM |
12PM-7PM |
7AM-Noon |
7AM-5PM |
3PM-11PM |
7AM-Noon |
7AM-5PM |
11PM-7AM |
7AM-Noon |
11AM-9PM |
Off |
7AM-Noon |
11AM-9PM |
12PM-7PM |
7AM-Noon |
11AM-9PM |
3PM-11PM |
9AM-Noon |
11AM-9PM |
11PM-7AM |
7AM-Noon |
1PM-11PM |
Off |
9AM-Noon |
1PM-11PM |
12PM-7PM |
9AM-Noon |
1PM-11PM |
11PM-7AM |
9AM-Noon |
11PM-7AM |
Off |
7AM-9AM |
11PM-7AM |
11PM-7AM |
7AM-9AM |
|
|
|
|
|
|
|
|
|
Every effort will be made to allow residents maximum conference attendance without compromising patient care.
Off-service Rotations:
For non-KCH sites and off-service rotations, please refer to the Clinical Responsibilities section of this handbook under the specific rotation heading for specific schedule information. In general, on the non-ED off-service rotations during the first two years residents will act as full members of the off-service clinical staff and have similar clinic and call schedules. For all off-service rotations at KCHC, excluding the SICU rotation, the resident is expected to attend conference for at least 2 hours – this is a required part of education and should be excused by the off-service team.
If the resident encounters a problem with the off-service schedule or conference attendance, the resident should first present this to the site director at the affiliate hospital. If the resident continues to have difficulty with this issue, the resident will present their difficulties to the chief residents who will facilitate the problem or refer the matter to the EM residency directors.